Surgical site infections - Annual Epidemiological Report 2016 [2014 data]
Executive Summary
Surgical site infections are among the most common healthcare-associated infections and are associated with longer post-operative hospital stays, additional surgical procedures, treatment in an intensive care unit, and higher mortality. These infections occur after an operation, in the part of the body where the surgical procedure was performed.
The latest ECDC annual epidemiological report on surveillance of surgical site infections in Europe show that hip prosthesis was the most frequently reported type of operation, representing 34% of all operations notified in that timeframe.
Overall, the trend analyses for the period 2011-2014 showed a statistically significant decreasing trend for four types of operations: coronary artery bypass graft, knee prosthesis, caesarean section, and colon surgery. These decreasing trends might suggest that the prevention of surgical site infections for these procedures has improved and that surveillance, by contributing to raising awareness about these infections and their prevention, might have contributed to the observed improvements.
An increase in the percentage of surgical site infections following cholecystectomy operations was observed during 2011-2014. Nonetheless, it is possible that this trend mainly reflects improvements, in some EU/EEA countries, in the surveillance of surgical site infections after discharge from the hospital.
One essential step in the prevention of surgical site infections is to implement a national system for their surveillance, as such a system provides an overview of the specific national situation and allows healthcare authorities to identify priorities and implement effective prevention measures. In 2017, ECDC will continue to provide support and tools, such as an updated protocol and a free software package, to those EU/EEA countries that wish to establish or improve their national systems and networks for the surveillance of surgical site infections.
The report contains data for 2013 and 2014, received from 15 EU Member States and one EEA country.
Surgical site infections - Annual Epidemiological Report 2016 [2014 data]
English (234.86 KB - PDF)Key facts
- Surgical site infections (SSIs) are among the most common healthcare-associated infections (HAI) [1]. They are associated with longer post-operative hospital stays, additional surgical procedures, treatment in intensive care units and higher mortality [2].
- In 2013–2014, 15 EU Member States and one EEA country reported SSIs for seven types of surgical procedure to ECDC.
- During this period, 18 364 SSIs were reported from a total of 967 191 surgical procedures.
- The percentage of SSIs per 100 surgical procedures varied from 0.6% to 9.5% depending on the type of procedure.
- The incidence density of in-hospital SSIs per 1000 post-operative patient-days varied from 0.2 to 5.7 depending on the type of surgical procedure.
- From 2011 to 2014, a significantly increasing trend was observed for the yearly percentage of SSIs in cholecystectomy operations.
- For coronary artery bypass grafts and knee prosthesis surgery, a significantly decreasing trend for both the yearly percentage of SSIs and the incidence density of SSIs was observed during 2011–2014.
Methods
Click here for a detailed description of the methods used to produce this annual report
SSI surveillance data for 2013–2014 were reported to ECDC by 16 countries (15 EU Member States and one EEA country). This report is based on data extracted on 6 April 2016.
Data on SSIs following surgical procedures that took place in 2013–2014 were collected in hospitals participating in national or regional surveillance of SSIs across Europe. The surveillance protocol allowed these hospitals to opt for patient-based or unit-based reporting [3]. SSI cases were classified according to the modified 2012 EU case definitions [4].
The SSI surveillance protocol includes seven types of surgical procedures: coronary artery bypass graft (CABG), cholecystectomy (CHOL), colon surgery (COLO), caesarean section (CSEC), hip prosthesis (HPRO), knee prosthesis (KPRO) and laminectomy (LAM). Only SSIs detected within a defined follow-up period were included in the analysis. For superficial SSIs, the follow-up period was 30 days. For deep or organ/space infections following orthopaedic operations with an implant in place (HPRO/KPRO), the follow-up period used in the analysis was 90 days (replacing the previous one-year period), reflecting the upcoming changes in the surveillance protocol [4,5,6].
For all patients with an SSI, basic demographics, infection characteristics and in-hospital outcome were collected. In the patient-based surveillance option, these data were collected from all surgical patients. Furthermore, information on each surgical procedure was collected, including whether the operation was urgent (i.e. not planned at least 24 hours in advance). The US National Healthcare Safety Network (NHSN) risk index, which is based on the presence of three major risk factors (duration of the operation, wound contamination class and the American Society of Anaesthesiologists (ASA) physical status classification), was used to assign all surgical patients to one of four categories (0 to 3) [7,8]. In this analysis, categories 2 and 3 were combined because of the low number of operations in these categories.
ECDC checked the reported SSI surveillance data for missing, unknown or discordant values and fed the results back to each country, which then had the option to correct the data.
For each type of surgical procedure under surveillance, two main indicators were calculated; the date of infection onset was used to determine if the SSIs were diagnosed during hospital stay:
• The percentage of SSIs per 100 operations: an indicator which includes both SSIs diagnosed during hospital stay and after discharge from the hospital (detected at hospital readmission or by post-discharge surveillance).
• The incidence density of in-hospital SSIs per 1 000 post-operative patient-days: an indicator which only includes SSIs diagnosed during hospital stay in patients with a known discharge date from the hospital.
For the patient-based data, both indicators were also stratified by NHSN risk index categories.
For each type of surgical procedure, trends in the percentage of SSIs and in the incidence density of SSIs between 2011 and 2014 were analysed by univariable Poisson regression. Given the dichotomous outcome, a robust sandwich variance estimator was used to correct the standard errors of the Poisson regression coefficients. Only countries that provided data using the same surveillance option (patient-based or unit-based) for at least three years were included in the trend analysis.
Epidemiology
Sixteen countries participated in the surveillance of SSIs. Thirteen countries and most of the United Kingdom (England, Northern Ireland and Wales) reported patient-based data whereas two countries and UK–Scotland reported unit-based data (Figure 1). The number of participating hospitals varied between countries, showing differences in the national coverage of the surveillance systems (Table 1).
Overall, 967 191 surgical procedures from 1 955 hospitals were reported in 2013–2014. Of these operations, 898 172 were reported using the patient-based surveillance and 69 019 using the unit-based surveillance (Table 1). The most common surgical procedure types under surveillance were HPRO operations (n=329 766), followed by KPRO operations (n=201 197) and CSEC operations (n=199 546).
Table 1. Number of reporting hospitals and reported surgical procedures by country and type of operation, EU/EEA, 2013–2014
|
Country |
Number of reporting hospitals |
No. of procedures |
No. of procedures |
No. of procedures |
No. of procedures |
No. of procedures |
No. of |
No. of procedures |
Total |
|---|---|---|---|---|---|---|---|---|---|
|
Patient-based data |
|||||||||
|
Austria |
48 |
954 |
1 133 |
389 |
8 390 |
11 703 |
3 229 |
|
25 798 |
|
Estonia |
1 |
304 |
|
|
469 |
|
|
|
773 |
|
Finland |
13 |
|
|
|
|
13 712 |
11 642 |
|
25 354 |
|
France |
345 |
1 159 |
18 010 |
7 649 |
28 936 |
31 465 |
10 387 |
2 417 |
100 023 |
|
Germany |
845 |
24 955 |
33 955 |
16 800 |
39 093 |
102 209 |
51 863 |
8 010 |
276 885 |
|
Hungary |
53 |
402 |
7 188 |
1 350 |
7 591 |
2 909 |
1 980 |
1 727 |
23 147 |
|
Italy |
126 |
2 588 |
13 379 |
9 194 |
18 470 |
5 176 |
2 507 |
1 998 |
53 312 |
|
Lithuania |
23 |
946 |
1 760 |
592 |
2 883 |
960 |
549 |
|
7 690 |
|
Malta |
1 |
384 |
|
|
400 |
573 |
792 |
|
2 149 |
|
Netherlands |
67 |
|
8 673 |
6 647 |
10 717 |
13 893 |
9 946 |
806 |
50 682 |
|
Norway |
59 |
4 198 |
8 880 |
6 205 |
18 668 |
22 323 |
|
|
60 274 |
|
Portugal |
37 |
49 |
5 509 |
3 006 |
3 400 |
3 031 |
2 357 |
1 070 |
18 422 |
|
Slovakia |
8 |
|
1 145 |
|
|
|
|
|
1 145 |
|
UK–England |
259 |
11 982 |
295 |
6 517 |
|
95 997 |
85 951 |
6 935 |
207 677 |
|
UK–Northern Ireland |
11 |
|
|
|
11 420 |
3 609 |
2 795 |
804 |
18 628 |
|
UK–Wales |
17 |
|
|
|
15 277 |
5 695 |
5 241 |
|
26 213 |
|
Subtotal |
1 913 |
47 921 |
99 927 |
58 349 |
165 714 |
313 255 |
189 239 |
23 767 |
898 172 |
|
Unit-based data |
|||||||||
|
Czech Republic |
1 |
|
|
566 |
|
|
|
|
566 |
|
Romania |
8 |
254 |
2 695 |
2 116 |
653 |
17* |
|
1087 |
6 822 |
|
UK–Scotland |
33 |
|
|
|
33 179 |
16 494 |
11 958 |
|
61 631 |
|
Subtotal |
42 |
254 |
2 695 |
2 682 |
33 759 |
16 511 |
11 958 |
1 087 |
69 019 |
|
EU/EEA |
1 955 |
48 175 |
102 622 |
61 031 |
199 546 |
329 766 |
201 197 |
24 854 |
967 191 |
Source: Country reports from Austria, the Czech Republic, Estonia, Finland, France, Germany, Hungary, Italy, Lithuania, Malta, the Netherlands, Norway, Portugal, Romania, Slovakia and the United Kingdom (England, Northern Ireland, Scotland and Wales)
* Excluded from further analysis because fewer than 20 surgical procedures of this type were reported by this country.
CABG: coronary artery bypass graft, CHOL: cholecystectomy, COLO: colon surgery, CSEC: caesarean section, HPRO: hip prosthesis surgery, KPRO: knee prosthesis surgery, LAM: laminectomy
.
Patient characteristics per surgical procedure type were only available for the patient-based data. The ratio of male to female patients was the highest in CABG operations (4.0) and the lowest in CHOL, HPRO and KPRO operations (0.6), excluding CSEC operations (0) (Table 2). The median age of patients varied from 31 years in CSEC operations to 72 years in HPRO operations. The post-operative in-hospital case fatality (4.1%), and the proportion of contaminated or dirty operations (30.4%) were the highest among COLO operations. The median duration of operation was the longest in CABG operations (199 minutes), and the median length of post-operative stay was the longest (8 days) in CABG and COLO operations. The proportion of urgent operations varied from 2.1% in KPRO operations to 54% in CSEC operations. In all surgical procedure types, apart from CHOL operations, more than 80% of patients received antibiotic prophylaxis. Of CHOL operations, 76% were reported as endoscopic operations compared with 26% of COLO operations.
Table 2. Characteristics of patients by surgical procedure type, patient-based data, EU/EEA, 2013–2014
|
Characteristics |
CABG |
CHOL |
COLO |
CSEC |
HPRO |
KPRO |
LAM |
|---|---|---|---|---|---|---|---|
|
Surgical procedures (n) |
47 921 |
99 927 |
58 349 |
165 714 |
313 255 |
189 239 |
23 767 |
|
Sex ratio (male:female) |
4.0:1 |
0.6:1 |
1.0:1 |
0:1 |
0.6:1 |
0.6:1 |
1.1:1 |
|
Median age (years) |
69 |
56 |
69 |
31 |
72 |
70 |
56 |
|
Post-operative in-hospital case fatality (%) |
1.6 |
0.5 |
4.1 |
0.0 |
1.5 |
0.2 |
0.2 |
|
Contaminated or dirty operations (%) |
0.5 |
15.4 |
30.4 |
6.3 |
1.3 |
0.7 |
0.9 |
|
Median duration of operation (minutes) |
199 |
60 |
140 |
37 |
75 |
79 |
80 |
|
Median length of post-operative stay (days) |
8 |
3 |
8 |
4 |
7 |
5 |
4 |
|
Urgent operations (%) |
8.7 |
17.4 |
18.2 |
53.6 |
10.5 |
2.1 |
5.2 |
|
Antibiotic prophylaxis (%) |
97.4 |
48.3 |
90.2 |
84.6 |
97.2 |
98.2 |
87.8 |
Source: Country reports from Austria, Estonia, Finland, France, Germany, Hungary, Italy, Lithuania, Malta, the Netherlands, Norway, Portugal, Slovakia and the United Kingdom (England, Northern Ireland and Wales).
See Table 1 for reporting hospitals and reported surgical procedures in EU/EEA countries.
CABG: coronary artery bypass graft, CHOL: cholecystectomy, COLO: colon surgery, CSEC: caesarean section, HPRO: hip prosthesis surgery, KPRO: knee prosthesis surgery, LAM: laminectomy
In 2013–2014, 18 364 SSIs were reported using patient- and unit-based surveillance. Of these, 10 288 (56%) were superficial, 4 722 (26%) deep and 3 318 (18%) organ/space SSIs. In 36 (0.2%) SSIs, the type of SSI was unknown. The proportion of deep or organ/space SSIs was 18% in CSEC operations, 33% in CHOL operations, 48% in COLO operations, 48% in LAM operations, 52% in CABG operations, 62% in KPRO operations and 67% in HPRO operations (Figure 2). Forty-one per cent of the SSIs were diagnosed in hospitals, whereas 53% were detected after discharge; for 6% the discharge date was unknown. The proportion of SSIs diagnosed in-hospital varied from 15% in CSEC operations to 67% in COLO operations.
Data on microorganisms were reported for 7 114 (38.7%) SSIs from 13 countries using patient- or unit-based surveillance. Overall, Staphylococcus aureus (17.0%) and Escherichia coli (16.9%) were the most commonly reported microorganisms (Table 3). The distribution of microorganisms varied by surgical procedure type. For CHOL and COLO operations, the majority of the reported microorganisms were Enterobacteriaceae. For all other surgical procedure types, gram-positive cocci were the most commonly reported microorganisms.
The percentage of SSIs varied by surgical procedure type (Fig.2):
For CABG operations, the percentage of SSIs was 3.0%, with an inter-country range from 2.4% to 6.7%.
For CHOL operations, the percentage of SSIs was 1.8%, with an inter-country range from 0.7% to 6.0%.
- In endoscopic CHOL operations, the percentage of SSIs was 1.5%, with an inter-country range from 0.4% to 5.6%.
- In non-endoscopic CHOL operations, the percentage of SSIs was 4.2%, with an inter-country range from 0.8% to 12.0%.
For COLO operations, the percentage of SSIs was 9.5%, with an inter-country range from 4.0% to 16.1%.
- In endoscopic COLO operations, the percentage of SSIs was 7.3%, with an inter-country range from 2.7% to 10.3%.
- In non-endoscopic COLO operations, the percentage of SSIs was 10.7%, with an inter-country range from 4.5% to 17.1%.
For CSEC operations, the percentage of SSIs was 2.2%, with an inter-country range from 0.6% to 7.7%.
For HPRO operations, the percentage of SSIs was 1.1%, with an inter-country range from 0.3% to 3.8%.
For KPRO operations, the percentage of SSIs was 0.6%, with an inter-country range from 0.0% to 3.4%.
For LAM operations, the percentage of SSIs was 0.7%, with an inter-country range from 0.1% to 2.1%.
Trend analysis of the yearly percentage of SSIs showed an increasing trend for CHOL operations (p<0.001) and a decreasing trend for CABG (p<0.001), CSEC (p<0.001), KPRO (p<0.001) and LAM operations (p=0.018) in 2011–2014 (Figure 3). For COLO and HPRO operations, no significant trend was observed in 2011–2014.
Similarly, incidence density of in-hospital SSIs varied by surgical procedure type (Fig. 3):
For CABG operations, the incidence density of in-hospital SSIs was 1.6, with an inter-country range from 0.6 to 11.4.
For CHOL operations, the incidence density of in-hospital SSIs was 1.5, with an inter-country range from 0.7 to 9.1.
- In endoscopic CHOL operations, the incidence density of in-hospital SSIs was 0.8, with an inter-country range from 0.3 to 2.3.
- In non-endoscopic CHOL operations, the incidence density of in-hospital SSIs was 3.2, with an inter-country range from 0.3 to 7.8.
For COLO operations, the incidence density of in-hospital SSIs was 5.7, with an inter-country range from 2.9 to 8.8.
- In endoscopic COLO operations, the incidence density of in-hospital SSIs was 4.5, with an inter-country range from 2.5 to 6.4.
- In non-endoscopic COLO operations, the incidence density of in-hospital SSIs was 6.0, with an inter-country range from 2.6 to 9.8.
For CSEC operations, the incidence density of in-hospital SSIs was 0.7, with an inter-country range from 0.0 to 2.5.
For HPRO operations, the incidence density of in-hospital SSIs was 0.5, with an inter-country range from 0.1 to 1.8.
For KPRO operations, the incidence density of in-hospital SSIs was 0.2, with an inter-country range from 0.0 to 1.7.
For LAM operations, the incidence density of in-hospital SSIs was 0.5, with an inter-country range from 0.0 to 2.7.
Trend analyses of yearly incidence density of in-hospital SSIs showed a decreasing trend for CABG (p<0.001), COLO (p=0.004) and KPRO operations (p<0.001) in 2011–2014, although for CABG operations the incidence density of in-hospital SSIs remained roughly the same during 2011–2013 before decreasing only in 2014 (Figure 4). No significant trends were observed for CHOL, CSEC, HPRO and LAM operations in 2011–2014.
Data on microorganisms were reported for 7 114 (38.7%) SSIs from 13 countries using patient- or unit-based surveillance. Overall, Staphylococcus aureus (17.0%) and Escherichia coli (16.9%) were the most commonly reported microorganisms (Table 4). The distribution of microorganisms varied by surgical procedure type. For CHOL and COLO operations, the majority of the reported microorganisms were Enterobacteriaceae. For all other surgical procedure types, gram-positive cocci were the most commonly reported microorganisms.
Table 3. Percentages of microorganisms identified in SSIs by surgical procedure type, pooled data from 13 EU/EEA countries, 2013–2014 (n=9 858)
|
Microorganisms |
CABG (n=1 059) |
CHOL (n=743) |
COLO (n=4 066) |
CSEC (n=528) |
HPRO (n=2 507) |
KPRO (n=814) |
LAM (n=141) |
Total (n=9 858) |
|---|---|---|---|---|---|---|---|---|
|
Gram-positive cocci |
61.0 |
35.1 |
31.1 |
50.0 |
65.3 |
69.2 |
61.0 |
47.9 |
|
Staphylococcus aureus |
19.4 |
9.8 |
4.3 |
25.8 |
30.8 |
34.4 |
29.1 |
17.0 |
|
Coagulase-negative staphylococci |
33.2 |
2.8 |
2.1 |
10.0 |
18.8 |
22.7 |
18.4 |
12.1 |
|
Enterococcus species |
7.6 |
19.4 |
21.9 |
7.2 |
11.3 |
6.3 |
9.2 |
15.2 |
|
Streptococcus species |
0.3 |
3.0 |
2.4 |
5.7 |
3.5 |
3.8 |
3.5 |
2.8 |
|
Other Gram-positive cocci |
0.5 |
0.1 |
0.3 |
1.3 |
1.0 |
2.0 |
0.7 |
0.7 |
|
Gram-positive bacilli |
1.2 |
0.7 |
0.4 |
1.5 |
2.2 |
2.8 |
0.7 |
1.2 |
|
Gram-negative bacilli, |
23.5 |
45.8 |
48.5 |
32.8 |
18.7 |
15.4 |
22.7 |
34.1 |
|
Escherichia coli |
4.3 |
22.1 |
28.6 |
17.4 |
6.1 |
4.1 |
9.2 |
16.9 |
|
Citrobacter species |
2.1 |
2.8 |
2.0 |
0.9 |
0.4 |
0.4 |
1.4 |
1.5 |
|
Enterobacter species |
4.5 |
5.8 |
4.6 |
3.8 |
3.2 |
3.2 |
0.7 |
4.1 |
|
Klebsiella species |
4.6 |
10.4 |
5.0 |
3.6 |
2.2 |
2.3 |
5.0 |
4.4 |
|
Proteus species |
3.9 |
1.9 |
3.2 |
4.2 |
3.5 |
2.6 |
3.5 |
3.3 |
|
Serratia species |
1.3 |
0.7 |
0.6 |
0.6 |
0.7 |
0.9 |
2.1 |
0.8 |
|
Other Enterobacteriaceae |
2.7 |
2.2 |
4.5 |
2.3 |
2.7 |
2.0 |
0.7 |
3.3 |
|
Gram-negative non- |
6.3 |
5.9 |
9.1 |
4.7 |
6.0 |
6.5 |
9.9 |
7.3 |
|
Acinetobacter species |
0.5 |
2.0 |
0.5 |
0.2 |
0.7 |
0.7 |
1.4 |
0.7 |
|
Haemophilus species |
0.2 |
0.1 |
0.0 |
0.6 |
0.0 |
0.1 |
0.0 |
0.1 |
|
Pseudomonas aeruginosa |
4.5 |
3.8 |
7.8 |
3.0 |
4.3 |
4.3 |
8.5 |
5.8 |
|
Pseudomonadaceae family, other |
0.7 |
0.0 |
0.2 |
0.2 |
0.8 |
0.6 |
0.0 |
0.4 |
|
Stenotrophomonas maltophilia |
0.4 |
0.0 |
0.1 |
0.0 |
0.1 |
0.5 |
0.0 |
0.2 |
|
Other gram-negative non- |
0.1 |
0.0 |
0.3 |
0.8 |
0.1 |
0.2 |
0.0 |
0.2 |
|
Anaerobes |
1.4 |
3.4 |
4.3 |
4.7 |
1.2 |
1.1 |
3.5 |
2.9 |
|
Bacteroides species |
0.3 |
1.6 |
3.5 |
1.7 |
0.5 |
0.2 |
0.0 |
1.8 |
|
Other anaerobes |
1.1 |
1.7 |
0.8 |
3.0 |
0.7 |
0.9 |
3.5 |
1.0 |
|
Other bacteria |
5.5 |
7.7 |
3.6 |
5.3 |
6.0 |
4.9 |
1.4 |
4.9 |
|
Fungi, parasites |
1.0 |
1.5 |
3.0 |
0.9 |
0.4 |
0.1 |
0.7 |
1.7 |
|
Candida species |
1.0 |
1.3 |
2.8 |
0.9 |
0.4 |
0.0 |
0.7 |
1.5 |
|
Other fungi or parasites |
0.0 |
0.1 |
0.2 |
0.0 |
0.0 |
0.1 |
0.0 |
0.1 |
Source: Country reports from the Czech Republic, Estonia, France, Germany, Hungary, Italy, Lithuania, Malta, the Netherlands, Portugal, Romania, Slovakia and the United Kingdom (England).
See Table 1 for reporting hospitals and reported surgical procedures in EU/EEA countries.
Discussion
The results of SSI surveillance presented in this report constitute a useful source of information on SSIs in the participating EU/EEA countries in 2013–2014. The number of reported surgical procedures and reporting countries remained stable in comparison to the previous years. However, the observed inter-country variation and the fact that not all EU/EEA Member States participated, limits the extent to which the overall results can be considered to be representative of the overall EU/EEA situation. For example, some European countries, which according to the ECDC point prevalence survey reported a low proportion of SSIs in healthcare-associated infections, did not participate in SSI surveillance [1]. In addition, national representativeness and surveillance methods vary considerably from country to country, which makes it difficult to compare data across countries. Important factors influencing the percentage of SSIs are the length of the follow-up period after surgery and the differences in post-discharge surveillance methods, especially in those surgical procedures where a large proportion of SSIs are detected after hospital discharge. Inter-country comparisons should therefore use the incidence density of in-hospital SSIs, if possible.
Both percentage and incidence density of SSIs were highest in COLO operations and lowest in KPRO and LAM operations [5,6]. However, the risk of SSI differs between surgical procedure types because of the different population groups that undergo these operations and because of the different proportions of clean and contaminated operations for each operation type. Therefore, comparisons of SSI rates should be restricted to each surgical procedure type, which can then be compared across countries and years.
In 2011–2014, a statistically significant increasing trend was only observed in the percentage of SSIs in CHOL operations. There was no statistically significant trend in the incidence density of SSIs in CHOL operations, and increases were only observed in SSIs diagnosed after discharge from the hospital. It is thus possible that this trend merely reflects improvements in the post-discharge SSI surveillance in some EU/EEA countries.
The 2011–2014 surveillance data show statistically significant decreasing trends in SSIs associated with four other types of surgery. Three types of surgery also showed a decrease in the incidence density of in-hospital SSIs. The decrease in 2011–2014 in both percentage of SSIs and incidence density of in-hospital SSIs in CABG and KPRO operations suggests that the prevention of SSIs for these surgical procedures has improved, both in hospitals and during the post-discharge period.
A comparison of the 2011–2014 trends with those reported from EU/EEA countries for 2008–2011 shows a continuous downward trend in the percentage of SSIs in CSEC and KPRO operations and in the incidence density of in-hospital SSIs in COLO operations throughout the entire 2008–2014 timespan [5]. It is, however, important to note that the yearly trends in the indicators can also be affected by the different mix of hospitals that each year participate in SSI surveillance.
The percentages of SSIs in the EU/EEA associated with certain surgical procedures were in large part similar to those reported from the United States for 2006–2008, apart from the considerably higher EU/EEA rates for CHOL and COLO surgery [9]. The percentages of SSIs for CHOL operations in the EU/EEA were also higher than those reported from Turkey for 2005–2011 [10]. All participating EU/EEA countries reported higher percentages of SSIs for CHOL operations than the United States. There is no clear explanation for these differences because the data reported from the United States and Turkey include the same subgroups that are used for EU/EEA surveillance. The data on the proportion of endoscopic operations also offer no convincing explanation [9,10]. But since the average post-operative stay after CHOL operations is very short (median three days), the intensity of post-discharge surveillance could explain the higher proportions of SSIs after cholecystectomies in some EU/EEA countries.
Public health conclusions
Surveillance is one of the key components in the prevention of healthcare-associated infections and an important tool for monitoring the effectiveness of prevention and control measures [11]. In fact, surveillance of SSIs in participating EU/EEA countries may have been a factor in driving the observed improvements and decreasing trends. To further strengthen the surveillance of SSIs in Europe, ECDC will update the surveillance protocol in 2017, adding structure and process indicators for infection prevention and control. This will provide participating hospitals with an improved tool to compare their performance with similar hospitals, both nationally and internationally. These changes aim to increase the usefulness of SSI surveillance networks in EU/EEA countries and increase hospital participation across Europe.
Further efforts are needed to increase the representativeness of European SSI surveillance by extending surveillance to other EU/EEA countries. ECDC will continue to provide support to countries that want to establish or improve their national surveillance networks. In addition to the SSI protocol update, ECDC will introduce a free software package (HelicsWin.Net) for SSI surveillance and make it available to network coordination centres and hospitals in 2017. The Centre will also promote the possibility to collect SSI surveillance data for shorter periods of time in all EU/EEA countries in 2018.
References
- European Centre for Disease Prevention and Control. Point prevalence survey of healthcare-associated infections and antimicrobial use in European acute care hospitals. Stockholm: ECDC; 2013. Available from: http://ecdc.europa.eu/en/publications/Publications/healthcare-associated-infections-antimicrobial-use-PPS.pdf.
- Awad SS. Adherence to surgical care improvement project measures and post-operative surgical site infections. Surg Infect. 2012 Aug;13(4):234-7.
- European Centre for Disease Prevention and Control. Surveillance of surgical site infections in European hospitals – HAISSI protocol. Version 1.02. Stockholm: ECDC; 2012. Available from: http://ecdc.europa.eu/en/publications/Publications/120215_TED_SSI_protocol.pdf.
- Commission Implementing Decision 2012/506/EU of 8 August 2012 amending Decision 2002/253/EC laying down case definitions for reporting communicable diseases to the Community network under Decision No 2119/98/EC of the European Parliament and of the Council OJ L 262/1; 27.9.2012. Available from: http://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32012D0506&from=EN.
- European Centre for Disease Prevention and Control. Surveillance of surgical site infections in Europe 2010–2011. Stockholm: ECDC; 2013.
- European Centre for Disease Prevention and Control. Annual Epidemiological report 2014 – Antimicrobial resistance and healthcare-associated infections. Stockholm: ECDC; 2014.
- Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999 Apr;20(4):250-78; quiz 279-80. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/SSI_1999.pdf.
- National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) System report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004 Dec;32(8):470-85. Available from: http://www.cdc.gov/nhsn/pdfs/datastat/nnis_2004.pdf.
- Edwards JR, Peterson KD, Mu Y, Banerjee S, Allen-Bridson K, Morrell G, et al. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009 Dec;37(10):783-805.
- Leblebicioglu H, Erben N, Rosenthal VD, Sener A, Uzun C, Senol G, et al. Surgical site infection rates in 16 cities in Turkey: findings of the International Nosocomial Infection Control Consortium (INICC). Am J Infect Control. 2015 Jan;43(1):48-52.
- Zingg W, Holmes A, Dettenkofer M, Goetting T, Secci F, Clack L, et al. Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. Lancet Infect Dis. 2015 Feb;15(2):212-24.
Annex
List of tables in the Annex:
- Table A1. Percentage of missing values by TESSy variable and year, patient-based data, 2013–2014
- Table A2.1. Percentage of SSIs and incidence density of in-hospital SSIs after coronary artery bypass graft operations by country, EU/EEA, 2013–2014
- Table A2.2. Mean and percentile distributions of percentage of SSIs and incidence density of in-hospital SSIs after coronary artery bypass graft operations in hospitals stratified by NHSN risk index, EU/EEA, 2013–2014
- Table A3.1. Percentage of SSIs and incidence density of in-hospital SSIs after cholecystectomy operations by country, EU/EEA, 2013–2014
- Table A3.2. Mean and percentile distributions of percentage of SSIs and incidence density of in-hospital SSIs after cholecystectomy operations in hospitals stratified by NHSN risk index, EU/EEA, 2013–2014
- Table A4.1. Percentage of SSIs and incidence density of in-hospital SSIs after colon surgery by country, EU/EEA, 2013–2014
- Table A4.2. Mean and percentile distributions of percentage of SSIs and incidence density of in-hospital SSIs after colon surgery in hospitals stratified by NHSN risk index, EU/EEA, 2013–2014
- Table A5.1. Percentage of SSIs and incidence density of in-hospital SSIs after Caesarean sections by country, EU/EEA, 2013–2014
- Table A5.2. Mean and percentile distributions of percentage of SSIs and incidence density of in-hospital SSIs after Caesarean sections in hospitals stratified by NHSN risk index, EU/EEA, 2013–2014
- Table A6.1. Percentage of SSIs and incidence density of in-hospital SSIs after hip prosthesis operations by country, EU/EEA, 2013–2014
- Table A6.2. Mean and percentile distributions of percentage of SSIs and incidence density of in-hospital SSIs after hip prosthesis operations in hospitals stratified by NHSN risk index, EU/EEA, 2013–2014
- Table A7.1. Percentage of SSIs and incidence density of in-hospital SSIs after knee prosthesis operations by country, EU/EEA, 2013–2014
- Table A7.2. Mean and percentile distributions of percentage of SSIs and incidence density of in-hospital SSIs after knee prosthesis operations in hospitals stratified by NHSN risk index, EU/EEA, 2013–2014
- Table A8.1. Percentage of SSIs and incidence density of in-hospital SSIs after laminectomy operations by country, EU/EEA, 2013–2014
- Table A8.2. Mean and percentile distributions of percentage of SSIs and incidence density of in-hospital SSIs after laminectomy operations in hospitals stratified by NHSN risk index, EU/EEA, 2013–2014
_________
* The European Surveillance System (TESSy) is a system for the collection, analysis and dissemination of data on communicable diseases. EU Member States and EEA countries contribute to the system by uploading their infectious disease surveillance data at regular intervals.
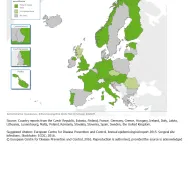
Participation in the surveillance of SSIs, EU/EEA, 2013–2014
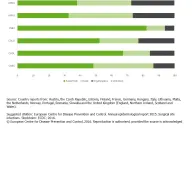
Types of SSI by surgical procedure type, EU/EEA, 2013–2014
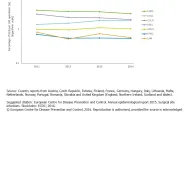
Trends of percentage of SSIs by year and surgical procedure type, EU/EEA, 2011–2014
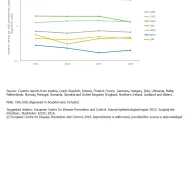
Trends of incidence density of in-hospital SSIs by year and surgical procedure type, EU/EEA, 2011–2014
Share this page
