COVID-19 testing strategies and objectives
Surveillance and monitoring
This document outlines strategies and objectives for sustainable SARS-CoV-2 testing of populations to achieve specific public health objectives in various epidemiological situations. General population-wide testing, as well as targeted testing of individuals, or specific populations related to particular settings, are presented on the basis of country experiences and information collected from scientific literature.
Executive Summary
Key messages
- Implementation of objective-driven and sustainable testing strategies for COVID-19 supports the overall public health response to the pandemic and helps mitigate its impact on vulnerable populations and healthcare systems, while ensuring that societies and economies can continue to function.
- ECDC proposes five main objectives for testing in order to control transmission; reliably monitor SARS-CoV-2 transmission rates and severity; mitigate the impact of COVID-19 in healthcare and social care settings; detect clusters or outbreaks in specific settings and maintain COVID-19 elimination status once achieved.
- Testing strategies should be flexible and rapidly adaptable to change, depending on the local epidemiology, transmission, population dynamics and resources.
- Ideally, all people with COVID-19 symptoms should be tested as soon as possible after symptom onset. This requires easy access to testing for all, including non-residents. Test turnaround time should be minimised, people testing positive should isolate and timely contact tracing should be carried out, ensuring that all close contacts are tested, irrespective of symptoms.
- All patients with acute respiratory symptoms in hospitals and other healthcare settings, and all specimens from sentinel primary care surveillance should be tested for both SARS-CoV-2 and influenza during the influenza season to monitor incidence and trends over time.
- Healthcare and social care settings require intensive testing when there is documented community transmission. Periodic and comprehensive testing of all staff and residents/patients is recommended to prevent nosocomial transmission. Furthermore, all patients/residents should be tested upon or immediately prior to admission.
- Clusters or outbreaks may occur in certain settings, such as workplaces, educational facilities, prisons, and migrant detention centres. Testing policies and systems should be in place for rapid detection and control to protect the relevant populations in these settings and to protect the community from amplified transmission.
- Countries experiencing high SARS-CoV-2 transmission in a local community should consider testing the whole population of the affected area. This would enable identification of infectious COVID-19 cases and allow for their prompt isolation to interrupt chains of transmission. Depending on the epidemiological situation, size and population density of the affected area, such an approach could be less disruptive for society than having to introduce and ensure compliance with more stringent public health measures.
- To prevent re-introduction, countries or sub-national areas that have achieved sustained control of SARS-CoV-2 circulation should, in addition to quarantine measures, consider targeted testing and follow-up of individuals coming from other areas within the same country, or from other countries that have not yet achieved sustained control of the virus.
Publication file
COVID-19 testing strategies and objectives
English (640.87 KB - PDF)Related content



Surveillance and monitoring


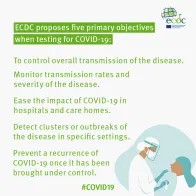
Infographic
Objectives for COVID-19 testing strategies
Share this page