Time to act and not react: how can the European Union turn the tide of antimicrobial resistance?
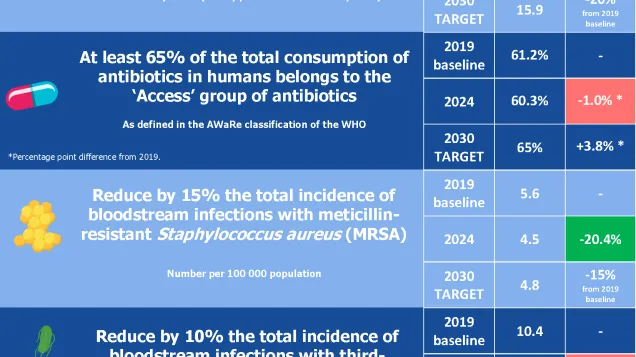
Despite determined efforts by countries and healthcare professionals, Europe is not on track to meet four of the five AMR targets set by the EU Council for 2030*.
Rising AMR, together with a shortage of novel effective treatments, constitutes an evolving major public health crisis in Europe and globally. In an interconnected world, AMR further complicates the health challenges that stem from non-communicable diseases, demographic shifts and healthcare workforce shortages.
‘Tackling AMR requires critical innovation on three key fronts: strong action for responsible antibiotic use, sustained and standardised infection prevention and control practice, and novel antibiotics in the pipeline’, says ECDC Director Dr Pamela Rendi-Wagner.
Europe is not on track to meet the 2030 AMR targets
Since 2019, the estimated incidence of bloodstream infections caused by carbapenem-resistant Klebsiella pneumoniae has increased by more than 60%, despite a target of 5% reduction by 2030. Similarly, those caused by third-generation cephalosporin-resistant Escherichia coli have risen by more than 5%, despite a target of 10% reduction.
Antibiotic consumption also increased in 2024, contrary to the 20% reduction target. Meanwhile, the proportion of first-line antibiotics used – those in the ‘Access’ group of the World Health Organization (WHO)’s AWaRe classification, which should represent at least 65% of total use – has remained stagnant at around 60%.
A human and societal crisis
ECDC estimates that antimicrobial-resistant infections cause more than 35 000 deaths every year in the EU/EEA, representing a substantial burden on individuals, societies and healthcare systems. The rise of resistant infections undermines modern medicine, jeopardising life-saving procedures like organ transplants, cancer therapy, surgery and intensive care.
‘Behind every statistic is a person whose treatment options are running out – a child, a parent, a grandparent. Antimicrobial resistance is not just a medical issue – it’s a societal one. We must ensure that no one in Europe is left without an effective treatment option,’ says Dr Diamantis Plachouras, Head of the Antimicrobial Resistance and Healthcare-Associated Infections at ECDC.
The perfect storm: rising AMR and shortage of effective treatments requires innovation
Several factors are contributing to the increase in difficult-to-treat infections: an ageing population with chronic underlying diseases that make them more vulnerable to infections, cross-border transmission of resistant microorganisms, and persistent high antibiotic use combined with gaps in infection prevention and control.
At the same time, the global antibiotic pipeline remains limited, especially against critical public health priority microorganisms like carbapenem-resistant gram-negative bacteria. Innovative solutions are needed to slow the rise of AMR, but there are very few new antibiotics offering novel mechanisms of action nearing approval.
Additionally, there is suboptimal use of first-line antibiotics from the ‘Access’ group of WHO’s AWare classification and growing dependence on last-resort antibiotics. These challenges highlight the need for coordinated action to secure equitable access, sustainable production, and responsible use of existing and future antibiotics.
ECDC’s role in supporting EU/EEA countries
ECDC continues to monitor AMR and antimicrobial consumption across Europe, assessing related public health risks and estimating the burden of resistant infections. The Centre works closely with EU/EEA countries to strengthen surveillance systems, enhance laboratory capacity, and leverage digital tools and electronic health records for better data-driven decision-making.
ECDC’s support to expand genomic surveillance of resistant pathogens has enabled earlier detection of emerging threats, improved outbreak tracking, and strengthened regional and global collaboration on AMR control. Tailored country support – through in-depth assessments of preparedness and response capacities for AMR and healthcare-associated infections – also ensures that all EU/EEA countries are better equipped to address this ongoing and evolving threat.
‘Antimicrobial resistance is an evolving challenge, but Europe can still make real progress. Together we can build a safer future, where effective treatment remains available for generations to come’, adds Dr Plachouras.
*A Council Recommendation adopted on 13 June 2023, outlines five targets related to antimicrobial consumption and resistance to be reached by 2030 by the EU and individual Member States, with 2019 as the baseline year.
EU Targets
-
Reduce the total consumption of antibiotics in humans by 20%;
-
At least 65% of the total consumption of antibiotics in humans comes from the ‘Access’ group of antibiotics in each country, as defined in the World Health Organization (WHO)’s AWaRe classification;
-
Reduce the total incidence of bloodstream infections with:
-
meticillin-resistant Staphylococcus aureus (MRSA) by 15%;
-
third-generation cephalosporin-resistant Escherichia coli (E. coli) by 10%;
-
carbapenem-resistant Klebsiella pneumoniae (K. pneumoniae) by 5%.
Latest reports



Watch videos of healthcare workers from Spain and Greece leading the change
Watch the recording of the digital event
Share this page