European standards of HIV prevention and care: Module on HIV and co-morbidities
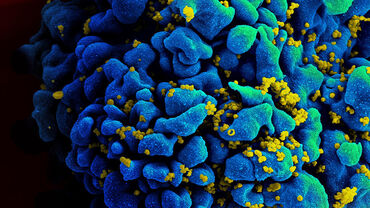
An estimated 2 334 662 people are living with HIV in Europe and Central Asia, of whom 1 944 695 have been diagnosed with the infection. As the population with HIV is aging, 18.7% of new HIV diagnoses occur in people aged over 50 years. Additionally, it is estimated that in Western and Central Europe, the proportion of people living with HIV aged 55 years and older will increase from 34% in 2020 to 47% in 2030.
With increasing life expectancy, people living with HIV face a growing burden of non-communicable diseases (NCDs), including cardiovascular disease (CVD), diabetes, cancers, chronic renal, liver, and pulmonary diseases, as well as mental and neurocognitive disorders. In the general population, the age-standardised mortality rate from NCDs in the World Health Organization (WHO) European Region was 427.1 (312.0–572.9) per 100 000 in 2019, with premature deaths accounting for 29.8% of cases, with people living with HIV experiencing an even higher burden of NCDs and increased mortality, as studies show that after 10 years of follow-up, individuals living with HIV have nearly twice the risk of developing an NCD (42.2% vs. 23.9% in the non-HIV cohort). By 2030, it is projected that up to 84% of people living with HIV will have at least one NCD, with 28% experiencing three or more.
The factors contributing to the higher prevalence of NCDs among people living with HIV are numerous and vary across countries and healthcare settings. Some are HIV-specific, such as persistent inflammation, late diagnosis, and antiretroviral therapy (ART)-related toxicities. Others, though common in the general population, may be more prevalent among those with HIV, including substance use, smoking, unhealthy diet, stigma and discrimination, barriers to care, and coinfections, all of which significantly impact NCD development and management.
The Sustainable Development Goals (SDG), adopted by the United Nations in 2015, emphasise the importance of ensuring healthy lives and promoting well-being for all ages. This includes the commitment to end AIDS, but also to ‘reduce by one-third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being’ by 2030. Achieving these goals requires a strong and standardised framework for HIV prevention and care across Europe.
Download

What are standards of care for HIV?
The standards of care (SoC) for HIV define the expected, or desired, quality of prevention, treatment, and care forpeople at risk of HIV acquisition or living with HIV.
The standards are based on a scientific rationale, as well as the responsibilities of each stakeholder and ensure that people receive appropriate, high-quality prevention and care that aligns with the most up-to-date medical knowledge and ethical standards.
The European Centre for Disease Prevention and Control (ECDC) in partnership with the European AIDS Clinical Society (EACS) have developed standards of care in the areas of HIV testing, pre-exposure prophylaxis (PrEP), antenatal screening, commencement of ART, and HIV and co-morbidities (add links to SoC modules). Each standard is based on the following structure:
1. Brief description of the rationale for the standard.
2. Quality statements describing best practice based on current guidelines, evidence, and expert opinion.
3. related measurable and auditable outcome indicators used to assess the quality and effectiveness of the services.
4. Numeric values for defined targets.
The standards are person-centred in their approach with a specific focus on being equitable, non-discriminatory, relevant, appropriate, and accessible for people at risk of or living with HIV.