Nipah virus disease
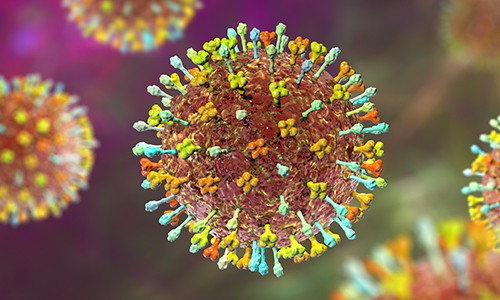
Nipah virus (Henipavirus nipahense) is a zoonotic pathogen. Its reservoirs are fruit bats or flying foxes (bats in the Pteropus genus), which are distributed at the coastal regions and in several islands in the Indian ocean, India, south -east Asia and Oceania. The virus can be transmitted to humans from wild and domestic animals. So far, outbreaks have only been reported in Asia; however, as the disease can be transmitted by domesticated animals and secondary human-to-human transmissions are also possible, it has considerable epidemic or pandemic potential.
Infections of humans with the Nipah virus may remain asymptomatic.
Clinical manifestation of acute Nipah virus disease may include:
- fever
- headache
- muscle pain
- nausea
- vomiting
- sore throat
- cough
- respiratory discomfort
- encephalitis (dizziness, drowsiness, altered state of consciousness and any other indicative neurological signs)
Travellers to or residents of Nipah virus endemic areas can be posed to the risk of Nipah virus infections mainly through direct or indirect contact with infected animals.
As symptoms during the first phase are not specific, early diagnosis is difficult, athough sensitive and specific laboratory methods exist.
In severe cases, encephalitis and convulsions occur, which can lead to coma and death. The mortality rate is between 40% and 75%, depending on the strain of the virus.
The virus is transmitted by direct contact with infected people or animals, or by contact with their body fluids. It can also occur through handling or eating contaminated food and through aerosols.
There is no proof that certain groups such as pregnant women, babies, or those with weak immune systems are more seriously affected. Spending longer time around those who are sick increases the risk of getting infected.
There are no specific treatment or vaccines available for the Nipah virus disease, either for people or animals. However, possible specific treatment options continue to be developed and evaluated.
In countries where cases exist, guidelines include supportive treatment in hospitals if necessary, and treatment for fever and convulsions.
Protective measures include guidelines to limit the spread of the disease both in households and hospitals (use of protective equipment, isolation, and safe contact with medical staff).
The options to prevent secondary transmissions are active case finding, contact tracing, isolation and quarantine of cases and their contacts.




