Spread of multidrug-resistant Shigella in EU/EEA among gay, bisexual and other men who have sex with men
The cases are linked to seven national and international distinct microbiological clusters, with chains of transmission largely, but not exclusively, among gay, bisexual and other men who have sex with men (gbMSM). Cases have been reported in Belgium (26), Denmark (13), Germany (33), Ireland (50), the Netherlands (21), Spain (> 60), and the United States (106). Most cases have been recorded during the period 2022−2023, but some date back to 2016.
An increase in extensively drug-resistant Shigella sonnei infections among gbMSM was already noted during the period 2020−2022 (see ECDC’s Rapid Risk Assessment dated 23 February 2022).
All strains in these seven clusters show resistance to first and second-line antibiotics, such as third-generation cephalosporins, fluoroquinolones, sulfamethoxazole, and trimethoprim. Of particular concern is resistance to azithromycin in some of the strains related to these clusters, as this limits the options for effective treatment.
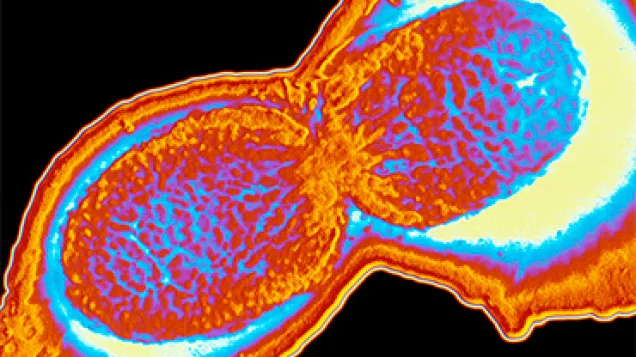
Infection and symptoms
Shigellosis is a gastrointestinal infection caused by Shigella bacteria. It is caught by ingesting material contaminated by human faeces, via direct oral-anal (or person-to-person) contact or hands/objects which have been in contact with faeces. The infective dose is extremely small, 10−100 organisms, making shigellosis easily transmissible. Infection can also result from contaminated food or water. Symptoms include acute diarrhoea, often accompanied by fever, abdominal pain and the presence of blood in stools. Most infections are self-limiting, lasting around 5−7 days, and do not require antimicrobial treatment. Treatment decreases the duration of symptoms by 1−2 days and may reduce the likelihood of onward transmission. Severe infection can also occur, especially in immunocompromised patients.
The risk of further transmission of shigellosis and other sexually transmitted infections (STIs) among gbMSM increases with the number of sexual contacts − e.g. during Pride and other international events. Spread of shigellosis among gbMSM also increases the risk of infection for their close contacts outside the gbMSM community.
Prevention and control
To minimise the risk of acquiring Shigella infection during sexual activity, it is recommended to practice safer sex and ensure good personal hygiene.*
If a person develops gastrointestinal symptoms, it is recommended that they refrain from sexual activity, pay extra attention to personal hygiene and seek healthcare to get tested for gastrointestinal pathogens and other STIs. It is important to inform the physician that the infection may have been acquired through sexual activity. People with gastrointestinal symptoms should not handle or prepare food in catering establishments, and should avoid using public pools, spas and hot tubs while they have gastrointestinal symptoms.
Furthermore, gbMSM who have been diagnosed with shigellosis should avoid sexual activity for at least seven days after symptoms have completely disappeared and oral-anal contact during sex for four to six weeks, given that Shigella can be shed in stools for up to six weeks. In addition, sexual partners of patients diagnosed with shigellosis should be notified and encouraged to contact a healthcare provider, in particular if they work in settings requiring close interaction with the general public (e.g. healthcare, child-care, food catering establishments) or if they develop symptoms of infection.
It is important to increase awareness among clinicians and microbiology laboratories of the international spread of multidrug-resistant Shigella bacteria and to ensure antimicrobial susceptibility testing of Shigella for cases of gastroenteritis in gbMSM, in order to guide antimicrobial treatment. Physicians should be aware that among young adult males the route of acquisition can be sexual (especially among those without travel history to a country with known increased risk of shigellosis). It is essential to report shigellosis cases to public health authorities and send Shigella isolates to national reference laboratories in order to monitor the development of antimicrobial resistance and enable the early detection and investigation of treatment failures. These should be reflected in updates of national and international treatment guidelines.
*The appropriate use of protective measures against Shigellosis infection among the gbMSM community includes disposable gloves for fingering or fisting, dental dams during oral-anal sex, as well as changing condoms between anal and oral sex. It is recommended to not share sex toys and to ensure proper cleaning and disinfection after their use and between partners. It is also important to wash hands, genital and anal areas before and after sexual contact.
Information on clinical management and prevention
More detailed information on clinical management and prevention practices can be found in the following documents:
The Health Protection Surveillance Centre in Ireland, 15 June 2023. Recommendation on aspects of management of shigellosis in Ireland in the context of current antimicrobial resistant Shigella species associated with gay, bisexual and men who have sex with men (gbMSM).
US CDC Health Advisory, 24 February 2023. Increase in Extensively Drug-Resistant Shigellosis in the United States.
ECDC Rapid Risk Assessment, 23 February 2022. Increase in extensively-drug resistant Shigella sonnei infections among men who have sex with men.
Share this page