Salmonella and Campylobacter show significant levels of resistance to common antimicrobials in humans and animals
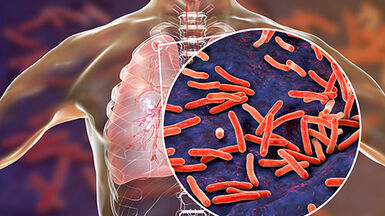
Treatment options for some of the most common food-borne infections are decreasing, as types of bacteria (called ‘isolates’) continue to show resistance to antimicrobial drugs. For example, multi-drug resistant isolates of Salmonella continue to spread across Europe. Also, high resistance to the antimicrobial ciprofloxacin in Campylobacter isolates in both humans and animals has been reported in some Member States. Encouragingly, co-resistance to critically important antimicrobials for both bacteria remains low. These are some the findings of the latest EFSA-ECDC European Union Summary Report on antimicrobial resistance (AMR) in zoonotic and indicator bacteria from humans, animals and food, which analyses data from 2013.
Treatment options for some of the most common food-borne infections are decreasing, as types of bacteria (called ‘isolates’) continue to show resistance to antimicrobial drugs. For example, multi-drug resistant isolates of Salmonella continue to spread across Europe. Also, high resistance to the antimicrobial ciprofloxacin in Campylobacter isolates in both humans and animals has been reported in some Member States. Encouragingly, co-resistance to critically important antimicrobials for both bacteria remains low. These are some the findings of the latest EFSA-ECDC European Union Summary Report on antimicrobial resistance (AMR) in zoonotic and indicator bacteria from humans, animals and food, which analyses data from 2013.
For the first time, EFSA and ECDC have used similar criteria to interpret data. “Findings in antimicrobial resistance in humans, animals and foods are now more comparable. This is a step forward in the fight against antimicrobial resistance”, said Marta Hugas, Acting Head of EFSA’s Risk Assessment and Scientific Assistance Department.
“The high levels of resistance to fluoroquinolones observed in Campylobacter isolates from both humans and broilers are of concern considering that a large proportion of human Campylobacter infections come from handling, preparation and consumption of broiler meat. Such high resistance levels reduce the effective treatment options for severe human Campylobacter infections”, said Mike Catchpole, Chief Scientist at ECDC.
Key findings
- Resistance in Salmonella to commonly used antimicrobials was frequently detected in humans and animals (especially broilers and turkeys) and derived meat products. Multi-drug resistance was high (in humans 31.8%, in broilers 56.0%, in turkey 73.0%, and in fattening pigs 37.9%), and the continued spread of particularly multi-drug resistant clones reported in both human and animal (broilers, pigs and cattle) isolates is of concern.
- Resistance to commonly used antimicrobials in Campylobacter isolates was frequently detected in humans and animals (especially broilers, pigs and cattle). In food, resistance was detected in broiler meat. Resistance to ciprofloxacin, a critically important antimicrobial, was particularly high in humans (meaning that treatment options for serious infections with these zoonotic bacteria are reduced). In Campylobacter jejuni more than half of both human and broiler isolates (54.6% and 54.5% respectively) were resistant, alongside 35.8% in cattle. In C. coli two thirds of humans and broiler isolates (66.6% and 68.8% respectively) were resistant along with 31.1% of pig isolates.
- Levels of co-resistance to critically important antimicrobials in Salmonella were low (in humans 0.2%, in broilers 0.3%, and in fattening pigs and in turkey there was none). Levels of multi-drug resistance and co-resistance in Campylobacter isolates to critically important antimicrobials were generally reported at low to moderate levels in animals (in C. jejuni isolates from broilers and cattle 0.5% and 1.1%, respectively, in C. coli isolates from broilers and fattening pigs 12.3% and 19.5%, respectively) and at low levels in humans (1.7% in C. jejuni and 4.1% in C. coli).
The report also includes data on resistance in indicator Escherichia coli, indicator enterococci and methicillin-resistant Staphylococcus aureus, in animals and food.
Note to editors
- EFSA and ECDC monitor AMR in humans, animals and food. This is the key to understanding how resistance develops and spreads. In its 2011 action plan against the rising threats from AMR, the European Commission identified key priority areas, including improved monitoring of antimicrobial resistance, to which this joint report 60makes an important contribution.
- AMR is resistance of a bacterium to an antimicrobial drug to which it was previously sensitive.
- Bacteria are multidrug-resistant if they are resistant to at least three different antimicrobial classes. In this report, co-resistance refers to combined resistance to two specific critically important antimicrobials.
- In previous reports, different interpretative criteria were used to establish the levels of microbiological resistance (resistance reported in animals and foods) and clinical resistance (resistance reported in humans). Criteria used to assess ‘microbiological resistance’ are often more sensitive than those used to assess ‘clinical resistance’. In this year’s report, criteria to assess microbiological resistance are used for both, animals and humans. Therefore, levels of microbiological resistance reported in humans are often greater than those reported in previous years.
- EFSA and ECDC have analysed the information submitted by 28 EU Member States on antimicrobial resistance in 2013. EFSA has been analysing resistance to antimicrobials in zoonotic bacteria found in animals and food since 2004.
For media enquiries please contact:
EFSA Media Relations Office
- Tel. +39 0521 036 149
- Email: Press@efsa.europa.eu
ECDC Press Office
- Tel. +46 (0)8 586 01 678 80
- Email: press@ecdc.europa.eu