ECDC releases risk assessment with actions needed to address spike in hepatitis A cases
The European Centre for Disease Prevention and Control (ECDC) has issued a Rapid Risk Assessment in response to a multi-country outbreak of hepatitis A in the EU/EEA. A significant increase in hepatitis A virus (HAV) infections has been reported in Austria, Czechia, Hungary, and Slovakia between January and May 2025. The rise in HAV infections is primarily affecting adults experiencing homelessness, individuals who use or inject drugs, and those living in poor sanitary conditions who have limited access to healthcare. Cases have also been reported among members of the Roma communities in both Czechia and Slovakia.
This outbreak reminds us that hepatitis A can cause serious illness and death, especially among people with limited access to healthcare and basic hygiene. We need to strengthen outreach, provide access to vaccination in groups more likely to be exposed, and ensure basic sanitation, especially in response to the increase in cases. More than health measures, they are equity measures.
said Ole Heuer, Head of Unit for One Health Related Diseases at ECDC.
The four affected countries have reported 2097 cases of hepatitis A in 2025. Slovakia – which has been experiencing an ongoing outbreak since late 2022 - has reported 880 cases reported in 2025 alone. This year, Austria has recorded 87 confirmed cases, including three deaths, already exceeding its 2024 total. In Czechia, 600 cases have been confirmed in 2025, including six deaths, with young children being the most affected group. Hungary has reported 530 cases this year, mainly among adults. Germany, though not considered an affected country, identified three cases with genomic profiles matching those in Hungary and Austria.
Genetic sequencing suggests ongoing person-to-person transmission within connected social networks or geographical areas, rather than multiple unrelated outbreaks. These findings confirm cross-border transmission and underscore the need for coordinated public health action, as well as the importance of collaboration, timely detection, and targeted interventions.
In EU/EEA countries currently experiencing outbreaks, the probability of sustained transmission and circulation of the virus is high among people living in poor sanitary conditions, people who inject drugs, and people experiencing homelessness. Because the severity of hepatitis A increases with age, the risk for these groups is considered high for adults aged 40 and above. For those with existing liver disease or older adults, the risk can be very high.
ECDC recommends EU/EEA public health authorities undertake a combination of actions including epidemiological investigations, targeted prevention, and community-based outreach to contain the outbreak and protect public health:
- Continuing to investigate hepatitis A transmission routes and increasing sequencing to understand the full epidemiological picture.
- Targeted vaccination of population groups more likely to be exposed to the virus should also be considered. Post-exposure prophylaxis using the hepatitis A vaccine should be prioritised for close contacts of identified cases according to national guidelines.
- Ensuring that people more likely to be exposed have easy access to basic hygiene such as soap and water in areas accessible to them such as public restrooms, homeless shelters, food banks.
- Tailor outreach activities to populations more likely to be exposed based on an understanding of their needs, attitudes and knowledge. Provide information in multiple languages, adapted to different literacy levels, and address rumours and misinformation that may be circulating.
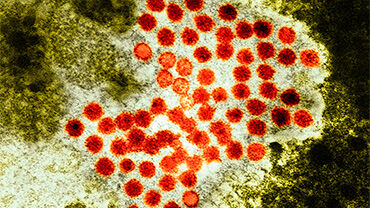
Hepatitis A is an acute viral liver disease caused by the hepatitis A virus (HAV), transmitted primarily via contaminated food, water, or close contact with infected individuals. It is a vaccine-preventable disease that most commonly affects people living in areas with poor sanitation or inadequate access to basic hygiene. Risk factors for infection include lack of access to safe water, close contact with infected individuals (including certain sexual behaviours such as anogenital-oral sex), use of recreational drugs, and travel to areas where the virus circulates. The likelihood of developing symptomatic or severe hepatitis A increases with age and is higher among people who are immunosuppressed or have chronic liver disease.
Read the report
Assessment
Rapid Risk Assessment: Multi-country outbreak of hepatitis A in the EU/EEA
This rapid risk assessment provides an overview of a multi-country hepatitis A outbreak in the EU/EEA during early 2025, highlighting its impact on vulnerable populations and identifying two closely related virus strains across affected regions.