Collaborating for Hepatitis C Elimination: Insights from Professor Loreta Kondili
Professor Loreta Kondili, a prominent public health expert based at the Italian National Institute of Health, is a leading figure in the fight against hepatitis C. She has dedicated her career to advancing research, shaping policy, and implementing strategies for disease elimination. Her work focuses on improving access to care and addressing barriers to treatment, particularly for vulnerable populations. In this interview, Ms Kondili shares her perspectives on key lessons, regional efforts, and collaborative strategies essential for achieving the WHO's hepatitis C elimination targets.
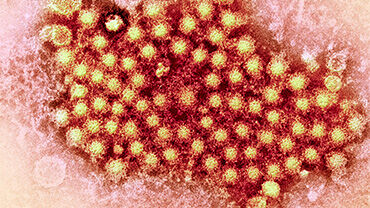
What is Hepatitis C, and why is it a public health concern?

Hepatitis C is a liver infection caused by the hepatitis C virus (HCV). It can also lead to extrahepatic complications such as vasculitis, cryoglobulinemia, diabetes, atherosclerosis, kidney problems, and psychiatric disorders. One major challenge is that it is often asymptomatic or manifests vague symptoms until severe liver damage, like cirrhosis or liver cancer, develops. Alarmingly, 40–74% of HCV-infected individuals experience at least one extrahepatic complication during their illness.
HCV is primarily spread through contact with infected blood. Before the virus was identified in 1991, transfusions of infected blood were a major transmission route. Today, risk factors include sharing syringes and inadequate sterilisation of medical or cosmetic instruments. While the highest infection rates are among drug users, cases also occur in the general population due to poorly sterilised medical or aesthetic procedures.
Scientific advancements have made significant strides in combating HCV. Diagnostic tools and direct-acting antiviral drugs (DAAs) can now cure HCV within 2–3 months with minimal side effects. This unprecedented success underpins the World Health Organization’s goal of eliminating HCV globally by 2030. Achieving this requires increasing diagnosis and treatment rates to significantly reduce new infections and liver-related deaths.
What are some of the main challenges that countries face in trying to eliminate hepatitis C?
Countries face several challenges in eliminating hepatitis C, spanning different stages of disease control and prevention. A critical first step is ensuring that individuals diagnosed with chronic HCV receive timely treatment to prevent disease progression and viral replication. However, access to treatment remains a significant hurdle, particularly for vulnerable populations with low health literacy. Many people do not know what steps to take due to the disease’s asymptomatic nature or the complexity of healthcare systems. Language and cultural barriers, as well as a lack of healthcare coverage for undocumented migrants, further complicate access to care. Stigma and discrimination also discourage affected individuals from seeking treatment.
Addressing these challenges requires decentralising services, running outreach programmes, task-sharing with non-healthcare providers, and offering culturally and linguistically sensitive care.
Another key issue is raising awareness. Public campaigns must empower people to understand the risks and seek care, as many are unaware of the disease and the availability of effective treatments. Equally, healthcare professionals—particularly in primary care—need training to recognise HCV as a cause of liver disease and severe comorbidities. They also need to understand the critical importance of linking patients to care and achieving a quick, effective cure. A multifaceted approach is essential to overcome these interconnected challenges and eliminate hepatitis C.
Could you describe some of the key strategies and actions being taken in the region to combat hepatitis C?
While EU countries provide universal access to DAA drugs, prescriptions are often restricted to specialists, complicating treatment access and care linkage. Many countries have prioritised key populations such as people who use drugs, inmates, and those co-infected with HIV. However, vulnerable groups like homeless individuals, people with mental health issues, migrants, refugees, and undocumented migrants are often underserved.
Successful outreach programmes targeting these populations in Spain, Italy, France, England, and Denmark have achieved excellent results in screening, diagnosis, and treatment. However, these initiatives are often sporadic and not fully integrated into national plans or healthcare systems. Countries need to harness the proven cost-effectiveness of HCV treatment, which offers short- and long-term benefits for individuals, society, and healthcare systems. Strengthening collaboration among stakeholders and affected communities is critical to expanding these efforts and achieving broader impact.
Are there lessons learned from Egypt’s hepatitis C elimination efforts that could benefit other countries?
Egypt is a clear example of what can be achieved with modern tools and strong political commitment. Once home to some of the highest rates of viral hepatitis globally, Egypt made remarkable progress through a comprehensive elimination programme. Key elements of its success included active screening, widespread awareness campaigns, and effective linkage to care initiatives.
The nationwide campaign offered routine testing to everyone over the age of 12 in healthcare facilities and through community outreach programmes. Teams visited markets, workplaces, sports clubs, mosques, churches, and even barbershops to ensure accessibility. Vulnerable groups, including refugees, migrants, and people with disabilities, were also included to leave no one behind. Egypt’s experience underscores the importance of inclusivity, outreach, and a holistic approach to fighting hepatitis C.
What opportunities in Europe today can be leveraged to accelerate hepatitis C elimination?
Most countries have developed national strategies focusing on raising awareness among at-risk groups to prevent new HCV infections, expanding treatment access, and implementing harm reduction measures. Modern diagnostic tools, telemedicine, and other IT solutions provide new opportunities to streamline care. Advanced diagnostic tests simplify and speed up HCV testing, reducing the need for multiple visits and improving linkage to care and treatment. Non-specialists, such as general practitioners and prison healthcare staff, can effectively manage screening and treatment, increasing accessibility. Successful micro-elimination efforts in target populations demonstrate the feasibility and cost-effectiveness of these approaches.
How does a workshop like this, organised under the EU Initiative on Health Security, contribute to the fight against hepatitis C?
Workshops like this are incredibly valuable for advancing hepatitis C elimination efforts. They provide a platform for sharing experiences, addressing challenges, proposing solutions, and learning from the successes of different countries. Specifically, this workshop fosters discussions on practical issues like improving access to care and reaching underserved populations.
Additionally, these workshops strengthen networks and foster collaborations among professionals across countries within and beyond the European region. Most importantly, they help define strategic actions tailored to regional needs, accelerating progress toward achieving the WHO's hepatitis C elimination targets.
Professor Loreta Kondili, MD, PhD, is a Senior Researcher at the Center for Global Health, Istituto Superiore di Sanità, and a member of the Policy, Public Health, and Advocacy Committee of the European Association for the Study of the Liver.