Pre-exposure prophylaxis for HIV prevention in Europe and Central Asia - Monitoring the implementation of the Dublin Declaration on partnership to fight HIV/AIDS in Europe and Central Asia: 2024 progress report (2023 data)
Executive summary
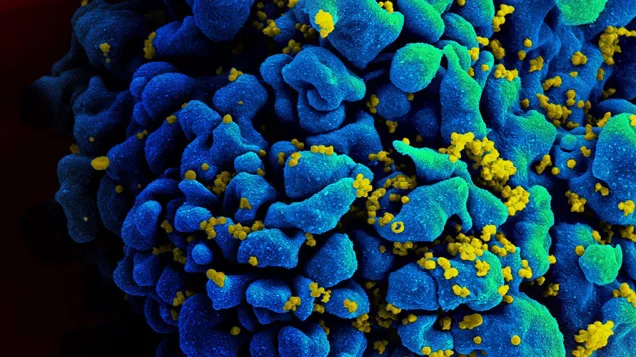
Pre-exposure prophylaxis (PrEP) is very effective at preventing HIV infection when taken as prescribed [1, 2]. It is an important element of the ‘combination prevention’ necessary to reach the United Nations (UN) Sustainable Development Goal of ending the AIDS epidemic by 2030 [3]. Since 2016, PrEP has been increasingly available through healthcare systems in the WHO European Region.
Between February and May 2024, the European Centre for Disease Prevention and Control (ECDC) implemented an online questionnaire among European and Central Asian countries to collect the most recent data as of 2023 to monitor the implementation of the 2004 Dublin Declaration [4]. The questionnaire contained specific questions on PrEP, in particular in relation to the availability of PrEP and on the uptake and cost of PrEP. This thematic report presents the results of the questionnaire, with a particular focus on equity of access amongst key populations.
While the provision of PrEP in Europe and Central Asia has increased significantly since 2016 [5], there is still a great deal of variation among countries in terms of the scale of implementation. By the end of 2023, 38 of 52 countries (23 EU/EEA countries) reported that national guidelines on PrEP had been developed and were being implemented, while 14 countries reported that guidelines on PrEP were either not developed (nine countries, of which five in the EU/EEA: Bulgaria, Cyprus, Hungary, Latvia, and Lithuania) or developed but not implemented (five countries, of which two in the EU/EEA: Greece and Romania). National PrEP guidelines are crucial for effective implementation. Countries without them should develop their own or adopt EACS guidelines, and address barriers where implementation is lacking. In the 34 countries in Europe and Central Asia which were able to report data, 284 846 people had received PrEP at least once in the last 12 months. Of these, 21 were EU/EEA countries (reporting a total of 153 799 people receiving PrEP at least once in 2023). This is far from the regional target to reach 500 000 people receiving PrEP at least once during the year by 2025 [6]. Sixteen of the 34 countries were able to provide data on the number of people using PrEP for the first time during the reporting period, with a total of 20 977 people being first time PrEP users. Of these, 12 were EU/EEA countries (reporting a total of 19 210 people as first time PrEP users).
However, even within countries reporting PrEP use, PrEP is not universally available, and some countries have restrictive eligibility criteria, especially for key populations like people who inject drugs, prisoners, and undocumented migrants. Progress has been made on increasing PrEP accessibility, with 12 countries (seven EU/EEA countries) also reporting PrEP being available to anyone at increased risk of HIV acquisition regardless of gender, sexual orientation, etc. To reach a wider population, we encourage countries to remove restrictions on who can access PrEP by making PrEP available to all individuals at increased risk of HIV acquisition. Among all people on PrEP in 19 countries (13 EU/EEA countries) able to provide data on PrEP use by key population, 10 countries (eight EU/EEA countries) reported that over 90% of the people accessing PrEP were men who have sex with men (MSM). Data on key populations accessing PrEP are very limited, especially for people who inject drugs (eight countries, of which four EU/EEA countries), migrants (seven countries, of which five EU/EEA countries), and prisoners (six countries, of which five EU/EEA countries), but the main barriers reported to scale-up PrEP are difficulties in reaching key populations and cost of PrEP to the individual. PrEP not being available in all parts or regions of the country, stigma and discrimination and long waiting list are also reported as barriers.
While some countries have reported PrEP availability in NGO/community-based settings, PrEP is still mainly provided in clinical settings, such as infectious disease clinics (27 of 43 countries, 19 EU/EEA countries). We encourage countries to expand PrEP access by exploring non-medical settings, like community-based organisations. Fourteen (eight in the EU/EEA) of the 43 countries reported that PrEP was available for free at public facilities, and eight (seven in the EU/EEA) reported that PrEP was free if the individual had insurance. Seven countries (six in the EU/EEA) reported that PrEP was only available at a cost, with the cost of a monthly supply of generic PrEP for an individual varying significantly across countries, ranging from €0 to €200 after reimbursement (median: €33) in 20 reporting countries. The median cost of one month’s supply of generic forms of PrEP in the sixteen EU/EEA reporting countries was €21.5 (range: €0 to €68) after reimbursement. Expanding the settings where PrEP is available may help improve accessibility. Sharing best practices especially those relating to feasibility, cost, and models of service delivery would support expanded provision of PrEP in the region.
Currently, data on PrEP uptake and unmet needs are limited across Europe and Central Asia. To better understand and address gaps in PrEP access among key populations, we encourage countries to strengthen surveillance systems and collect data on PrEP uptake. Strong surveillance systems should capture data on PrEP eligibility, uptake (by gender and key populations), duration, and outcomes. Consistent data collection across regions would improve comparability.
Pre-exposure prophylaxis for HIV prevention in Europe and Central Asia - Monitoring the implementation of the Dublin Declaration on partnership to fight HIV/AIDS in Europe and Central Asia: 2024 progress report (2023 data)
English (2.53 MB - PDF)Share this page