Mapping surveillance systems for HIV/AIDS in the EU/EEA 2025
Executive summary
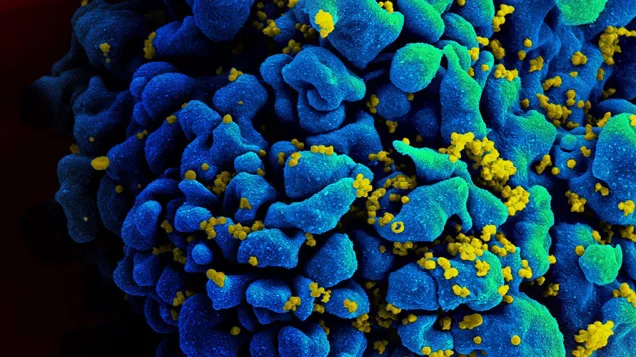
Effective surveillance is crucial for tracking HIV/AIDS trends, informing prevention efforts, and guiding healthcare planning. Routine HIV and AIDS data collection also supports risk analysis, incidence modelling, and policy development, while monitoring key sustainable development goal indicators, (such as SDG 3.3 – ‘End the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases)’. Regular evaluations ensure surveillance systems remain accurate, efficient, and sustainable. This survey mapped and analysed HIV/AIDS surveillance across European Union (EU) and European Economic Area (EEA) countries and identified gaps and areas for improvement.
The survey was based on the Outcome and Assessment of Surveillance Indicators and Systems (OASIS) methodology and adapted for HIV surveillance using a semi-quantitative tool with 107 questions to evaluate organisational and functional aspects. Organisational attributes assessed the structure and management of the surveillance system, including objectives, governance, resources, stakeholder involvement, and data management. Functional attributes evaluated acceptability, usefulness, representativeness, and timeliness in system performance. A questionnaire was distributed to nominated national focal points in each EU/EEA country, with responses stored in ECDC’s system.
Several areas for improvement were identified:
- Establish, regularly review and update surveillance objectives and protocols to ensure alignment with current public health priorities: the survey found that some EU/EEA countries have outdated HIV surveillance objectives and reporting protocols and a few other countries lack them entirely.
- Strengthen governance frameworks and enhance stakeholder engagement: there was an absence of a clearly defined governance structure or dedicated surveillance steering committee in some countries which limits effective coordination and decision-making. Addressing this would improve the overall impact of HIV surveillance.
- Improve technical infrastructure and advanced digital solutions: some countries reported gaps in secure electronic data transfer, system interoperability, and the integration of laboratory and epidemiological data, which hinders the efficiency and accuracy of HIV surveillance.
- Streamline reporting systems, enhance training, and provide stronger support for healthcare providers and staff in laboratories: most countries identified time constraints as the primary barrier to reporting. Some cited inadequate infrastructure, complex reporting processes, and insufficient training for clinicians and those working in laboratories as contributing factors to underreporting.
- Implement standardised approaches to measure and address underreporting: A high level of underreporting was noted by some countries; however, many countries reported not using any formal methodology to quantify its extent. There is a need to to ensure more accurate and representative surveillance.
- Make surveillance systems more adaptable, streamline data integration, and leverage new health technologies: Many countries struggle to collect key data such as death records, dates of death, AIDS diagnoses after an HIV diagnosis, and previous positive cases, revealing significant gaps in HIV surveillance.
- Regular evaluation and continuous improvement of surveillance systems: The lack of regular internal and external evaluations in several countries limits opportunities for performance improvement, showing the need for systematic assessment processes to ensure HIV surveillance systems remain effective, reliable, and adaptable.
Mapping surveillance systems for HIV/AIDS in the EU/EEA 2025
English (5.92 MB - PDF)Share this page