Efficacy, effectiveness and safety of HPV vaccination in women with conisation: a systematic review and meta-analyses
The objective of this review was to investigate the efficacy, effectiveness and safety of HPV vaccination in women undergoing conisation compared with those not receiving a HPV vaccination. HPV vaccination related to conisation was defined for the purposes of this study as HPV vaccine given shortly (i.e. four months or less) before, at or after conisation (as ‘adjuvant’ intervention to conisation, secondary prevention). We conducted meta-analyses separately for randomised controlled trial (RCTs) and non-randomised studies of the effects of interventions (NRSI).
Executive Summary
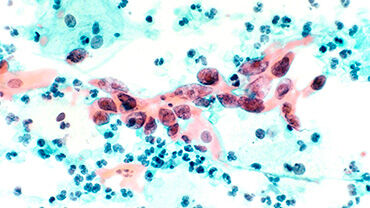
Cervical cancer is the fourth most common cancer affecting women worldwide. It is caused by persistent infection with oncogenic types of human papillomavirus (HPV). More than 200 types of HPV have been identified and more than 40 types of them infect the genital tract. HPV 16 and 18 are the two primary oncogenic types and are responsible for 71% of cervical cancers, and HPV 31, 33, 45, 52 and 58 together account for 18% of cervical cancers.
The review found that the use of HPV vaccines in comparison to not using them in women with conisation may reduce the risk of CIN 2+ and CIN3+ (both irrespective of HPV type) and CIN 2+ (related to HPV 16/18). However, confidence in the effect estimates is limited. The evidence on the effect of HPV vaccination in comparison to no vaccination on CIN3+ (related to HPV 16/18), invasive cervical cancer, persistent HPV infections (irrespective of HPV type) and persistent HPV infection (related to HPV 16/18) was very uncertain.
The evidence for the effect of HPV vaccine in women with conisation was inconclusive for the outcomes CIN 2, CIN 3, VIN 2+ and VaIN 2+ and mortality. There were no data available for incident HPV infections (irrespective of HPV type and related to HPV 16/18), AIS and quality of life. One RCT comparing vaccinated women with women who did not receive a vaccine reported severe allergies (two cases) and minor local reactions to the HPV vaccine. Subgroup analyses according to type of vaccine were only possible for CIN 2+ (irrespective of HPV type and related to HPV 16/18). No differences were identified.
Overall, the existing evidence related to the HPV vaccine in women with conisation is predominantly derived from NRSI with serious or critical risk of bias. Evidence from RCTs is very limited, i.e. only two RCTs are available. Further additional RCTs with a placebo intervention in the control group to evaluate the efficacy of HPV vaccines (particularly the nonavalent vaccine) as an adjuvant to conisation would provide more robust evidence. These RCTs should additionally consider the HPV vaccination status of the women concerned (in terms of primary prevention). Moreover, it would be crucial to extend follow-up times to the generation of robust data on the incidence of cervical cancer and cancer-related mortality.
Download