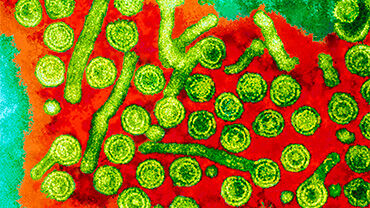
Hepatitis B vaccination policies, practices and challenges to achieving hepatitis elimination in the European Union and European Economic Area
This report provides an overview of current information on hepatitis B virus (HBV) vaccination among European Union (EU) and European Economic Area (EEA) countries. It highlights progress towards the 2025 interim targets related to vaccination that are defined in the World Health Organization (WHO) Regional action plans on ending AIDS and the epidemics of viral hepatitis and sexually transmitted infections (STIs) 2022–2030.
Executive summary
There are an estimated 3.2 million people living with chronic HBV infection across the EU/EEA. The prevalence of HBV infection has been falling globally due to the impact of vaccination and is now below 1% in most EU/EEA countries, but still exceeds 2% in a few countries. The prevalence of infection also remains high among some populations at increased risk of infection, including people in prison, people who inject drugs, men who have sex with men and some migrant populations. Another result of vaccination has been the steady fall over time in reported cases of acute hepatitis B infection, with very few cases now reported across countries which suggests that current transmission levels are low. However, recent data highlight an increase in reports of acute hepatitis B across the region, which may be related to factors such as changes in reporting and testing, but may also relate to an increase in local transmission.
Hepatitis B vaccination is recommended by all countries, but there is considerable variation in whether it is recommended as part of the childhood schedule, whether a birth dose of the vaccine is provided universally to all babies, or whether it is targeted to the babies of mothers with HBV infection. A total of 27 EU/EEA countries recommend universal hepatitis B vaccination as part of their routine childhood schedule, with most of these programmes established decades ago. However, of these countries, under half of them with available data were achieving the 2025 WHO interim target of 95% coverage with three doses of the childhood HBV vaccination. Additionally, in some countries, vaccination coverage has fallen in recent years. Five countries in the EU/EEA have implemented a universal birth dose of the HBV vaccine, with all of them reporting over 90% coverage with timely birth dose vaccination and meeting the WHO 2025 interim target. Countries had differing policies regarding vaccination of groups at higher risk of infection, with more countries having policies targeting healthcare workers and less with policies tailored to men who have sex with men, people who inject drugs, people in prison and certain migrant populations. Very limited data on vaccination coverage were reported for these groups and, where available, the coverage was low.
All countries across the region have programmes to prevent mother-to-child transmission. These include universal antenatal screening and several interventions for the mother and baby such as post-exposure prophylaxis to babies born to mothers with an HBV infection, including provision of a birth dose of the hepatitis B vaccine and hepatitis B immunoglobulin if indicated. Data collected from countries that provide a targeted birth dose of hepatitis B vaccine indicates high coverage, with three quarters of reporting countries reporting 100% coverage of the targeted birth dose.The prevalence of HBV infection among women screened antenatally is low and programmatic and surveillance data together suggest that current levels of mother-to-child transmission across countries in the region is very low.
Current priorities around HBV prevention include maintaining high coverage in HBV vaccination programmes and comprehensive programmes targeting the prevention of mother-to-child transmission, to minimise the number of infections occurring in infants. Achieving the WHO elimination targets related to HBV vaccination among children and the prevention of mother-to-child transmission are therefore important priorities for countries in their efforts to prevent and control hepatitis B. Efforts to understand what the gaps are in vaccination programmes in order to increase vaccination coverage are critical to ensure the population is well protected and future infections are prevented. This is especially important in light of the suspected increase in transmission of hepatitis B infection across the region. In countries with suboptimal vaccination coverage, it is important to assess factors that underlie low coverage, such as public perception toward vaccinations in order to develop tailored communication strategies and to identify any barriers to vaccination in the community such as restricted access or costs to the individual. Whilst current transmission of HBV is at a low level across the EU, there remain individuals who are increased risk of infection who are unvaccinated and a life-long approach to vaccination should be adopted using local epidemiological data to identify groups that should be prioritised for vaccination.