Testing of HIV, hepatitis B and hepatitis C in the European Union/ European Economic Area (EU/EEA)
Introduction and methods
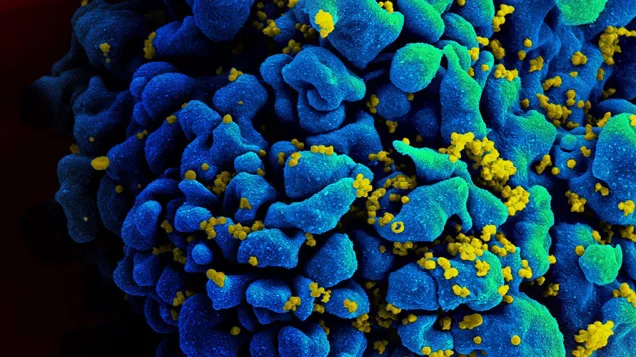
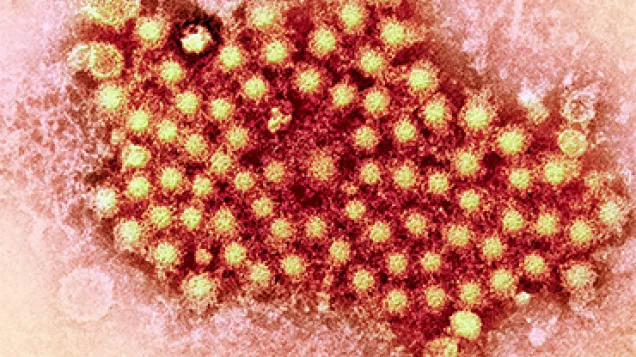
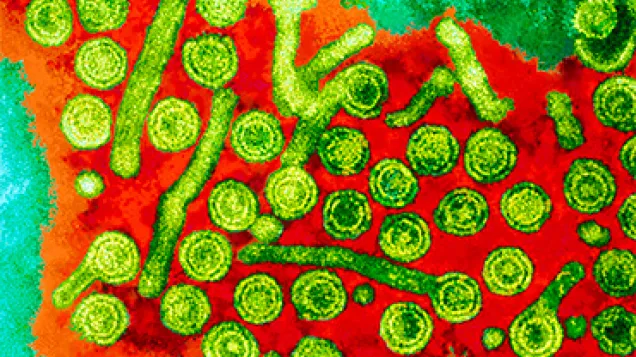
Timely and effective testing for HIV, hepatitis B virus (HBV) and hepatitis C virus (HCV) is essential to controlling these blood-borne viruses. Negative test results offer opportunities for prevention, including HIV pre-exposure prophylaxis (PrEP), condom provision and counselling, hepatitis B vaccination and harm reduction interventions for people who are at risk of blood-borne virus infection through injecting drug use. Global targets set by The United Nations Programme on HIV/Aids (UNAIDS) and the World Health Organization (WHO) aim to eliminate the epidemics of AIDS and viral hepatitis as public health threats by 2030.
This report summarises progress in European Union/European Economic Area (EU/EEA) countries towards implementing integrated testing strategies, based on the public health guidance on integrated HIV, hepatitis B and C testing published by the European Centre for Disease Prevention and Control (ECDC) in 2018. It draws on monitoring and surveillance data reported to ECDC in 2024 for HIV and in 2023 for hepatitis, covering the existence of national testing policy and guidance (and whether guidance is integrated across viruses and specific populations), the degree of guidance implementation, testing uptake and coverage, including late diagnoses and the percentage of people living with the three viruses who have been diagnosed.
Key findings on the integration of testing for HIV, HBV and HCV
Integration of testing guidance
Guidance included in national policy, strategy or recommendations on HIV, HBV and HCV testing is out of date in many EU/EEA countries and not aligned with ECDC recommendations.
- While 27 of 30 countries include HIV testing in national policy, only 17 have integrated recommendations for HIV, HBV, HCV and sexually transmitted infections (STIs).
- Over half of the countries have not updated their testing guidance since 2018 when ECDC’s guidance was published.
- For hepatitis, 22 of the 30 countries reported having a national plan or strategy covering the response to hepatitis.
Coverage of key populations:
ECDC recommends that testing for HIV, HBV and HCV is offered to key populations at increased risk of infection.
- Most countries include key populations in HIV testing guidance (27 of 30 countries), while somewhat fewer do so for HBV and HCV.
- Men who have sex with men (MSM) and people who inject drugs (PWID) are most commonly included; transgender people and people in prison are less frequently taken into consideration.
Testing approaches and accessibility
- For HIV, provider-initiated testing in primary and secondary care and community-based testing by trained medical providers are the most commonly implemented approaches, while home testing and testing in other healthcare settings, such as pharmacies, remain limited.
- For hepatitis, rapid HCV tests are available in the majority of EU/EEA countries but peer-to-peer testing (for HBV and HCV) is only available in one-third of the countries and self-tests for HCV remain rare.
- HIV, hepatitis B and C disproportionately affect marginalised populations who may find testing more acceptable when delivered in community settings by peers, referred to as ‘lay providers’. There are still restrictions on who can perform tests, with 22 countries requiring healthcare professionals for HIV and 23 for HBV/HCV.
- Testing is not universally free: only 24 countries offer free testing to all for HIV and 17 for hepatitis.
Testing coverage and outcomes
- Most countries lack testing data disaggregated by key population or setting for all three infections, which limits our understanding of availability and accessibility of testing among those who are most at risk. HIV positivity rates are higher in community settings than in healthcare settings. Data on testing volume and positivity by setting were available for about half of the countries for HIV but were not included in data collection for hepatitis.
- Over 50% of HIV cases are diagnosed late (CD4 count <350 cells/mm3 blood), with individuals probably living undiagnosed for 3–5 years posing them at increased risk of morbidity, mortality, worse treatment outcomes and transmitting the virus to others.
- For hepatitis, late-stage diagnoses with chronic HBV/HCV infection (with end-stage liver disease, including decompensated cirrhosis and/or hepatocellular carcinoma) are common, exposing those who are at risk to life-threatening complications.
- In terms of progress toward the global diagnosis targets, an estimated 92% of people living with HIV had been diagnosed in 26 EU/EEA countries with available data. Seven countries had met the 95% target and an additional eight were within 5% of the target. While the target of 95% of people living with HIV being aware of their HIV status may be feasible to achieve, reaching the WHO targets (60% of those with chronic hepatitis B and C being diagnosed) will be more challenging. For hepatitis, results on progress towards the WHO targets were available from just four countries, with none having met the 60% target for HBV and only three having met the 60% target for HCV.
Priorities for action
- Update national testing policies to reflect integrated, multi-disease approaches, ensuring alignment with ECDC guidance and global targets.
- Include recommendations on the testing of key populations in national guidance and expand integrated testing policies to include all key populations, especially those that are underserved.
- Diversify testing approaches, including peer-led and self-testing, to improve reach and acceptability, particularly outside traditional healthcare settings. Peer involvement, lay-provider testing, community outreach and culturally and linguistically tailored approaches (including mobile health and use of social media) are methods that are likely to increase access and engagement with testing services among key and vulnerable populations.
- Remove legal barriers to lay provider testing and ensure free access to testing, especially for vulnerable populations.
- Strengthen monitoring systems to capture testing uptake and outcomes by population and setting, enabling targeted improvements.
Testing of HIV, hepatitis B and hepatitis C in the European Union/ European Economic Area (EU/EEA)
English (1.76 MB - PDF)Share this page