A systematic review and meta-analyses of the efficacy, effectiveness, immunogenicity and safety of HPV vaccination in non-HIV immunocompromised individuals
The objective of this review was to investigate the efficacy, effectiveness, immunogenicity and safety of HPV vaccination in non-HIV immunocompromised individuals of any age.
Executive summary
Background
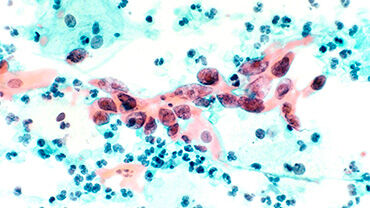
Cervical cancer is the fourth most common cancer affecting women worldwide. It is caused by persistent infection with oncogenic types of human papillomavirus (HPV). More than 200 types of HPV have been identified and more than 40 types of them infect the genital tract. HPV 16 and 18 are the two primary oncogenic types and responsible for 77% of cervical cancers (i.e. squamous cell carcinoma), and combined with HPV 31, 33, 45, 52 and 58, account for 94.9% of cervical cancers [1-3]. While HPV infections are common and usually resolve without any
consequences, persistent infections with high-risk HPV can progress to premalignant glandular or squamous intraepithelial lesions (cervical dysplasia).
HPV vaccination in adolescents is an important measure to prevent cancer [4, 5]. To date, most HPV vaccination programmes target adolescent girls and/or boys, while some countries have extended HPV vaccination catch-up programmes to adults [6]. In Europe, three HPV vaccines are currently approved: bivalent, quadrivalent and nonavalent. All three HPV vaccines include virus-like particles of the high-risk oncogenic HPV types 16 and 18, and the nonavalent HPV vaccine comprises the five additional (oncogenic) HPV types 31, 33, 45, 52 and 58.
Although HPV vaccination of adolescents showed beneficial effects in the general population, it is unclear whether and to what extent the HPV vaccine offers protection to an immunocompromised population, such as individuals with organ transplants, stem cell therapy or populations under immunomodulatory therapy. Immunocompromised individuals have a potentially higher risk for infectious diseases and certain cancers compared to the general population, and studies on HPV suggest that immunocompromised individuals are at an increased risk for HPV related diseases (e.g. cervical cancer) [7-12].
While existing evidence syntheses on HPV vaccination in immunocompromised individuals primarily focuses on populations with human immunodeficiency virus (HIV) [13-15], there is no comprehensive systematic review on other immunocompromised populations [16-18].
Objectives
The objective of this review was to investigate the efficacy, effectiveness, immunogenicity and safety of HPV vaccination in non-HIV immunocompromised individuals of any age.
Search methods
The systematic search was conducted on 6 May 2024 in three electronic databases: Ovid MEDLINE, Ovid Embase and the Cochrane Central Register of Controlled Trials (CENTRAL). The study registry ClinicalTrials.gov was also searched to identify ongoing studies or unpublished completed studies. No date or language restrictions were used.
Selection criteria
Randomised controlled trials (RCTs) and non-randomised studies of interventions (NRSI) were included. Studies included those investigating immunocompromised individuals, including primary or secondary immunodeficiencies and individuals under therapy, as defined in section 3.1.2. Studies on HIV and other infectious diseases (e.g. malaria or helminthiasis) were excluded of any age and sex. Studies included (i) nonavalent HPV vaccine, (ii) quadrivalent HPV vaccine and (iii) bivalent HPV vaccine.
Studies that were included compared a vaccinated immunocompromised group with any of the following groups:
- Unvaccinated immunocompromised control group with the same disease or condition (comparison 1);
- No vaccination;
- Placebo (containing no active agent, only the adjuvant of the HPV vaccine);
- A non-HPV vaccine.
In addition, the following groups were considered:
- Other vaccinated immunocompromised control group with a different disease or condition that affects the immune system (comparison 2);
- Other immunocompromised group who received the HPV vaccination;
- Vaccinated healthy control group (comparison 3);
- Healthy control participants from the general population who are not immunocompromised (as defined in section 3.3.1) who received the HPV vaccination
For safety/adverse outcomes data, studies without an independent comparison group (i.e. single-arm studies) were also included.
The following outcomes prospectively prioritised by the experts of the HPV Working Group were included:
- Patient relevant outcomes (for HPV type 16/18): Precancer or cancer of the cervix, precancers or cancers of
the vulva, vagina, penis or anus and oropharyngeal cancer; - HPV infection (for HPV type 16/18);
- Immunogenicity (for HPV type 16/18);
- Safety/adverse outcomes: Any serious adverse event (as defined by clinical trial authors).
Data collection and analysis
The results of random-effects meta-analyses for the primary analyses was used and the Hartung-Knapp adjustment in case of three or more studies was also applied. The risk of bias was assessed (with the ROBINS-I tool) and the certainty of evidence was rated using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach.
Results
Key characteristics of the included studies
A total of 27 reports were included with 23 NRSI contributing data to this systematic review. Overall, two studies were identified comparing a vaccinated immunocompromised group with an unvaccinated immunocompromised control group with the same disease or condition (comparison 1). Most included studies provided indirect evidence by comparing vaccinated immunocompromised participants to other vaccinated immunocompromised groups with a different disease or condition (comparison 2) (n=2), or to vaccinated healthy control groups (comparison 3) (n=14). Additionally, six single-arm studies were identified. Studies took place in Europe (n=4), North America (n=14), Australia (n=1), South America (n=2) and Asia (n=2) and were published between 2013 and 2023. Studies comprised a wide range of immunocompromised individuals including participants with allogeneic stem cell transplant, autoimmune diseases, Fanconi anemia, inflammatory bowel disease, juvenile idiopathic arthritis, juvenile dermatomyositis, systemic lupus erythematosus, survivors of cancer, and organ transplant recipients (e.g.
liver and kidney).
Summary of main results
Since variability in participant groups introduced substantial clinical heterogeneity, separate meta-analyses and certainty of evidence assessments for each participant group was conducted, thereby limiting the ability to perform further subgroup and sensitivity analyses, e.g. for sex, age, timing of the vaccination and specific immunosuppressive treatments.
Studies assessed patient relevant outcomes (as described in the methods) rarely. Only one NRSI, a case-control study, assessed precancer or cancer of the cervix (i.e. CIN 2+ and CIN 3+) comparing a vaccinated immunocompromised group to an unvaccinated immunocompromised control group. Hence, the effect of HPV
vaccination on CIN 2+ and CIN 3+ was of very low certainty. As a result, most of the review’s findings were based on the remaining comparisons – i.e. vaccinated immunocompromised participants compared to other vaccinated immunocompromised groups with a different disease or condition, or to vaccinated healthy control participants – reporting on immunogenicity data, predominantly measured at seven months after initial vaccination (seropositivity rates and geometric mean ratios [GMRs]), accompanied by limited safety data.
Overall, the certainty of evidence of immunogenicity and safety data was low to very low across all comparisons, primarily downgraded due to (very) serious risk of bias and (considerable) imprecision. All vaccinated immunocompromised groups (e.g. cancer survivors, juvenile idiopathic arthritis or systemic lupus erythematosus) demonstrated seroconversion rates (seropositivity) of 100 or nearly 100 percent and were similar to other vaccinated immunocompromised groups (comparison 2) or to vaccinated healthy control groups (comparison 3). Most immunocompromised groups had similar GMTs compared to healthy control groups (comparison 3) but the results were often imprecise, as the 95% confidence intervals frequently overlapped the null effect of GMR = 1, indicating effects that potentially vary.
Seropositivity rates and GMRs were comparable between different time points (i.e. 7 months and 12 months and more after first vaccination). All findings from meta-analyses remained robust under the fixed-effect model in sensitivity analyses.
SAEs (e.g. hospital admissions) were rare in the vaccinated groups and deemed unrelated to the HPV vaccine by the study authors. Common local adverse events across HPV vaccine types were pain, induration, erythema and edema, while systemic adverse events frequently included headache, fatigue and nausea.
Conclusions
Data on patient relevant outcomes (e.g. precancer or cancer of the cervix) are lacking. Most evidence relies on immunogenicity data and some safety outcomes from studies comparing vaccinated immunocompromised participants to other vaccinated immunocompromised groups with a different disease or condition, or to vaccinated healthy control participants. Overall, HPV vaccination appears to be immunogenic and generally safe across immunocompromised groups, considering that the data is of low to very low certainty of evidence. Due to the unclear correlate of protection (e.g. towards HPV-associated cancers) and lack of standardisation of assays and protocols for antibody measurement, it is important to interpret immunogenicity data with caution. Moreover, immunogenicity results may be influenced by various factors, including the underlying clinical conditions that affect the immune system, different immunosuppressive treatments, timing of the vaccine administration, prior exposure to HPV, as well as variations in age and sex. Thus, further research is needed to better differentiate between immunocompromised groups and subgroups.