World AIDS Day 2020: The way towards 2030: diversified testing to diagnose HIV early

On the occasion of World AIDS Day on 1 December each year, ECDC and the WHO Regional Office for Europe releases the latest data on the HIV epidemic in the European Region.
The good news on the way towards the 2030 target: the proportion of new HIV diagnoses per year across EU/EEA countries has declined by 9% since 2010 and the number of people living with undiagnosed HIV has been going down.
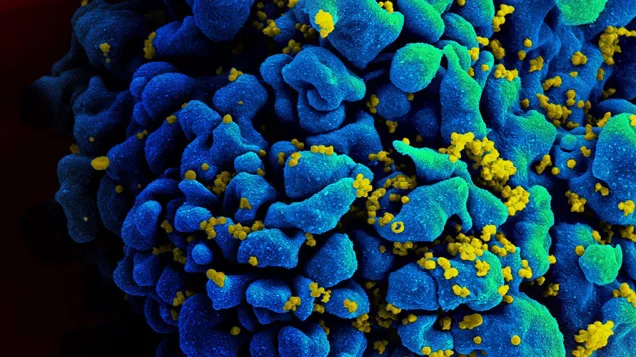
However, one trend, observed across Europe over the last decade, is that every second HIV diagnosis happens at a late stage of infection when the immune system has already started to fail. According to ECDC estimates, it takes on average three years from the time of HIV infection until diagnosis. Three years during which HIV positive people do not get live-saving treatment and during which they can unknowingly pass on HIV.
Late diagnosis suggests persistent problems with access to, and uptake of, HIV testing and counselling in many countries. If Europe wants to reduce the high proportion of people diagnosed late, it is essential to diversify HIV testing strategies as outlined in the ECDC testing guidance.
Early diagnosis of HIV is important as it allows quicker linkage to care and antiretroviral treatment. This in turn increases people’s chances of living a longer and healthier life. At the same time, effective treatment leads to an undetectable viral load – which means that those on effective HIV treatment cannot transmit the virus.
What can be done?
To reduce the future number of new HIV infections, Europe needs to focus on three main areas:
- Prioritising effective and comprehensive prevention measures such as awareness-raising; promotion of safer sex, condoms and substitution therapy, provision of needle exchange programmes and pre-exposure prophylaxis for HIV;
- Providing efficient HIV counselling and testing services, including rapid diagnostic services, community-based HIV testing and HIV self-testing; and
- Ensuring rapid access to quality treatment and care for those diagnosed.

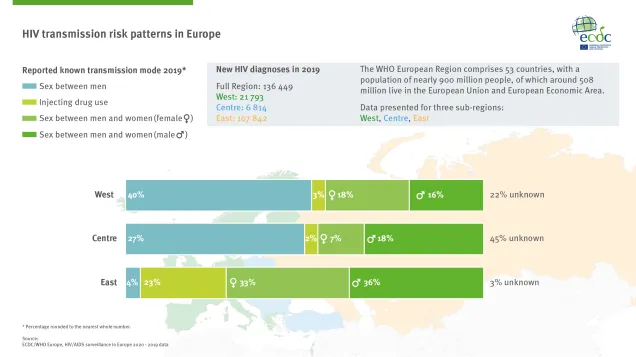
The number of people living with undiagnosed HIV is increasing in the WHO European Region. According to data published today by ECDC and the WHO/Europe, more than 136 000 people were newly diagnosed in 2019 – roughly 20% of these were diagnosed in the EU/EAA and 80% in the eastern part of the European Region. Every second HIV diagnosis (53%) happens at a late stage of the infection, when the immune system has already started to fail. This is a sign that testing strategies in the Region are not working properly to diagnose HIV early.

This report is the latest in a series published jointly by the European Centre for Disease Prevention and Control (ECDC) and the WHO Regional Office for Europe that has been summarizing data on HIV and AIDS in the WHO European Region and in the European Union and European Economic Area (EU/EEA) since 2007.
HIV/AIDS surveillance in Europe 2020
English (10.37 MB - PDF)
The coronavirus disease (COVID-19) continues to challenge healthcare systems across the World Health Organization (WHO) European Region. As World AIDS Day 2020 approaches, it serves as a reminder about the importance to maintain a strong HIV response at all levels. Further, as framed in the Sustainable Development Goals (SDGs) and recent European and global guidance, it is critical to approach testing for HIV, hepatitis B (HBV), hepatitis C (HCV), and sexually transmitted infections (STIs), namely chlamydia, syphilis and gonorrhoea, in an integrated and synergistic manner.
Share this page