Disease information on measles
Measles is an acute, highly contagious viral disease capable of causing epidemics. Infectivity is close to 100% in susceptible individuals and in the pre-vaccine era measles would affect nearly every individual during childhood. Immunisation has dramatically reduced the incidence of measles in Europe but despite overall high immunisation coverage, measles continues to cause frequent outbreaks. Measles remains one of the leading causes of death among children globally. The elimination of measles and rubella as well as the prevention of congenital rubella syndrome forms part of a global elimination goal. Progress towards elimination is being monitored on an annual basis through a European Regional Verification Commission for Measles and Rubella Elimination (RVC) established in 2011.
The pathogen
- The measles virus is a single-stranded RNA virus of the genus Morbillivirus and the family Paramyxoviridae.
- The virus is related to several viruses that infect animals, including the Canine Distemper Virus. Primates can be infected in vitro but humans are the only reservoir for the measles virus which, theoretically, could be eradicated from the world.
- The entire measles virus genome has been sequenced which has allowed for identification of distinct wild-virus lineages with different geographical distribution. This makes it possible to confirm or suggest the source of an outbreak.
- Vaccine induced immunity protects against all virus strains. Measles is considered a monotypic virus despite the genetic variations.
Clinical features and sequelae
- The prodrome starts after a 10–12-day incubation period and is characterised by fever, conjunctivitis, coryza, cough and bronchiolitis. Nearly all infected susceptible individuals develop clinical disease.
- Koplik’s spots, the enanthema believed to be pathognomic for measles, appear on the buccal mucosa 1–2 days before the onset of rash.
- The measles rash, an erythematous maculopapular exanthema, develops 2–4 days after the onset of fever and spreads from the head to the body over the next 3–4 days.
- The rash, which blanches on pressure early in the course, fades in the order of appearance during the next 3–4 days and assumes a nonblanching appearance.
- Mortality from measles is predominantly caused by complicating bacterial infections.
- Complications are likely to have developed if the fever does not drop within 1 or 2 days after the onset of the rash.
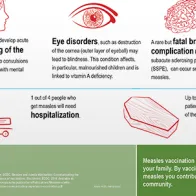
- The most common complications of measles are: otitis media (7–9%), pneumonia (1–6%), diarrhoea (8%), post-infectious encephalitis (1 per 1000 to 2000 cases), and subacute sclerosing panencephalitis (SSPE), which affects 1 per 100 000 cases.
- Case fatality is 1–3 per 1000 cases and highest in those younger than five years of age and among immunocompromised individuals. Pneumonia accounts for six out of ten measles associated deaths.
- Subacute sclerosing panencephalitis (SSPE) is a rare (1 per 100 000 cases) and fatal degenerative central nervous system disease caused by a persistent infection with a mutant measles virus. The onset is several years after the episode of measles (on average seven years) and most affected children had measles before two years of age.
- Infants are protected from birth against measles by maternal antibodies if the mother is immune to measles. This passive immunity gradually disappears over the second half of the first year of life. Infants with partial passive immunity may develop milder and shorter episodes of measles that still confers lasting immunity.
Epidemiology
- EU measles case definition for the purpose of epidemiological surveillance.
- In the pre-vaccine era, measles was endemic in Europe and most people would be infected during childhood. Regular outbreaks occurred at 2–5 year intervals in most populations, and few people would remain susceptible beyond 20 years of age.
- Immunisation against measles started in the 1960s and has dramatically changed the epidemiology of the disease. Measles is no longer endemic in most European countries but outbreaks resulting mainly from imported index cases remain common in countries where subgroups of the population have low levels of immunity.
- The annual number of confirmed measles cases in Europe has been in the thousands since 2001 and several countries experienced outbreaks in recent years.
- Routine measles immunisation in childhood leads to widening intervals between epidemics during which the group of susceptible individuals builds up.
- Humans are the only natural host of the virus and measles meets the following criteria for a disease that can be eradicated:
- No animal or environmental reservoir.
- Accurate diagnostic tests are available.
- The measles vaccine is highly effective and safe.
- Measles elimination in large geographic areas has been demonstrated.
- Global eradication of measles would occur when the last chain of transmission of measles virus is interrupted in every country.
- ECDC publishes monthly surveillance data on measles and rubella submitted by the 30 EU/EEA countries. ECDC also monitors European and worldwide measles outbreaks through epidemic intelligence and reports on them on a monthly basis in the Communicable Disease Threat Reports (CDTR)
Transmission
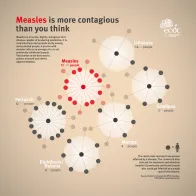
- Measles is extremely communicable and it is estimated that 90% of non-immune people exposed to an infective individual will contract the disease. Mathematical models estimate the basic reproductive number at 12–18; that is the average number of secondary infections that follow a single introduction into a susceptible population.
- The virus is transmitted from person to person via respiratory droplets produced when sick people cough and sneeze. Virus-containing droplets can remain in the air for several hours and the virus remains infectious on contaminated surfaces for up to two hours.
- Infected people are considered contagious from about five days before the onset of rash to four days afterwards. Measles is maximally contagious during the prodromal phase which lasts for 2–4 days and is characterised by intense coughing.
- Invasion is through the respiratory epithelium and 2–3 days after exposure there is a primary viremia with replication in the inoculation site as well as in distant reticuloendothelial tissue.
- On days 5–7, there is an intense secondary viremia of 4–7 days with replication in the skin, conjunctivae, respiratory tract and internal organs.
- Individuals at increased risk of measles include infants who are too young to be immunised, people in whom the vaccine has failed to induce immunity (primary vaccine failure), and individuals who for medical, religious or other reasons have not been immunised.
Prevention
- Immunisation is the only effective preventive measure against acquiring measles.
- The live attenuated measles vaccine induces an immune response that is similar to naturally acquired immunity and can be boosted by challenge from wild or vaccine virus.
- Measles vaccine is at least 95% effective and seroconversion rates are close 100%. Primary vaccine failure of the first dose at 12 months of age or older occurs in up to 5% of people, but 95% of first dose failures will seroconvert from a second dose.
- Maternal antibodies are the most common cause of primary vaccine failure. The age of first immunisation with measles vaccine must balance the chance of seroconversion with the risk of infection. This is why, in countries with endemic measles, the first dose of measles containing vaccine (MCV) is given as early as nine months, often complemented by another dose during the second year of life.
- Experience and modelling shows that two doses of measles vaccine is required to interrupt indigenous transmission and achieve herd immunity. A single dose in the second year of life will induce immunity in about 95% of immunised people. This means that 100% uptake would be required in order to achieve the desired 95% immunity level. However, about 95% of those who fail to respond to a first dose develop immunity from a second dose and hence the benefit of a second dose.
- All EU/EEA immunisation programmes recommend a two-dose measles immunisation schedule with the first dose given during the second year of life and the second dose at an older age that differs between countries. Catch-up programmes are in place for those who may have missed vaccination or who are uncertain about their vaccination history.
- Measles vaccine is administered as part of a combination of live attenuated vaccines that includes measles, mumps, rubella or measles, mumps and rubella. In some countries a combination vaccine that also includes the varicella antigen may be used.
- Combination vaccines have been shown to elicit the same immune response as individual vaccines. Vaccinating individuals who are already immune to one or more of the antigens in the combination vaccine, either from previous immunisation or natural infection, are not associated with any increased risk of adverse events.
- Regarding post-exposure prophylaxis, administration of an MCV is the intervention of choice within 72 hours of exposure is possible as the incubation period for vaccine virus is shorter than that for wild virus.
- The immunisation schedule for measles in the EU/EEA can be found in the ECDC Vaccine Scheduler.
Management and treatment
- Measles should be suspected in anyone who presents with an acute erythematous rash and fever preceded by cough, coryza, conjunctivitis and photophobia.
- Measles may in some cases be difficult to distinguish from other causes of febrile illnesses with rash, and infections with rubella, parvovirus B19, human herpes virus type 6 (HHV-6) and dengue can easily be mistaken for measles.
- Diagnosis relies on laboratory tests. All suspected measles cases should either be laboratory confirmed or epidemiologically linked to a confirmed case.
- There is no specific antiviral therapy for measles and most cases will recover with supportive treatment including hydration and antipyretics.
- Bacterial superinfections are common and should be treated with antibiotics but prophylactic treatment is not indicated. Continued fever beyond two days after the onset of rash is an indication of complications.
- Airborne transmission precautions are indicated for hospitalised patients for four days after the onset of rash.
- Management of exposed people should include immunisation with an MCV as it will provide protection in some cases if given within 72 hours of exposure.
- All cases of suspected measles should be reported to the relevant national health authority without waiting for the results of diagnostic tests.
- Active surveillance for measles and prompt implementation of response measures are essential components of the measles elimination strategy for Europe.
Note: The information contained in this fact sheet is intended for the purpose of general information and should not be used as a substitute for the individual expertise and judgement of healthcare professionals.