Antimicrobial resistance surveillance in Europe 2023 - 2021 data
Executive Summary
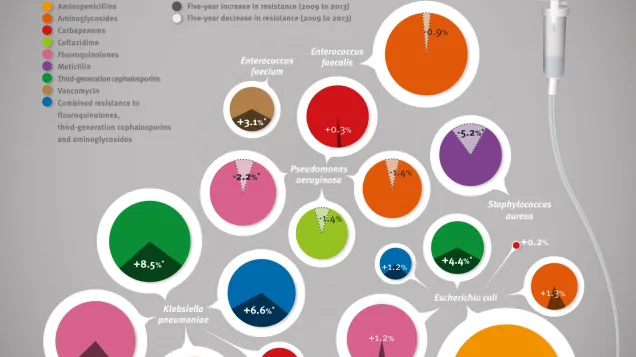
The AMR situation in bacterial species reported to the AMR surveillance networks referring to isolates obtained in 2021 varied widely depending on bacterial species, antimicrobial group and geographical region (see Fig. 1–10 in Chapter 3). Resistance to third-generation cephalosporins and carbapenems was generally higher in Klebsiella pneumoniae than Escherichia coli. While carbapenem resistance remained rare in E. coli for most countries, 33% of the countries reported resistance percentages of 25% or higher in K. pneumoniae. Carbapenem resistance was also common in Pseudomonas aeruginosa and Acinetobacter species, and at a higher percentage than in K. pneumoniae. As observed in previous regional reports, there is a north-to-south and west-to-east gradient of resistance, with higher rates observed in the southern and eastern parts of the European Region than in the northern and western parts. This was particularly evident for third-generation cephalosporin and carbapenem resistance in K. pneumoniae and carbapenem resistance in Acinetobacter spp.
Considering only the 13 countries that submitted data to CAESAR both in 2020 and 2021, the overall number of isolates reported was higher in 2021 than in 2020. This was a result of higher numbers of isolates being reported across all pathogens. These overall tendencies were not always observed at country level, however, all countries reported higher numbers of Acinetobacter spp. isolates in 2021 than in 2020. In all 16 countries submitting data to CAESAR in 2021, the majority of isolates (70.0%) were E. coli (37.9%), Staphylococcus aureus (17.2%) and K. pneumoniae (14.9%).
Looking at bacterial species-specific results in 2021,resistance to fluoroquinolones in E. coli was generally lowest in the northern parts of the WHO European Region and highest in the southern (see Fig. 1 in Chapter 3). A resistance percentage below 10% was observed in two (4%) of 45 countries reporting data on this microorganism. A resistance percentage of 25% or above was reported in 17 (38%) countries. A resistance percentage of 50% or above was observed in four (9%) countries. For third-generation cephalosporin resistance in E. coli, 12 (27%) of 45 countries reported percentages below 10%, whereas resistance percentages equal to or above 50% were observed in four (9%) (see Fig. 2 in Chapter 3). Eight (18%) of 44 countries reported carbapenem-resistant E. coli percentages of 1% or above (see Fig. 3 in Chapter 3).
Third-generation cephalosporin resistance in K. pneumoniae has become quite widespread in the WHO European Region. In 2021, percentages below 10% were observed in seven (16%) of 45 countries reporting data on this microorganism, while 19 (42%), particularly in the southern and eastern parts of the Region, reported resistance percentages of 50% or above (see Fig. 4 in Chapter 3). Carbapenem resistance was more frequently reported in K. pneumoniae than in E. coli. In 2021, resistance
percentages were generally low in the northern and western parts of the WHO European Region; 14 (31%) of 45 countries reported resistance percentages below 1% (see Fig. 5 in Chapter 3). Fifteen (33%) countries reported percentages equal to or above 25%, eight of which (18% of 45 countries) reported resistance percentages equal toor above 50%.
Large differences were observed in the percentages of carbapenem-resistant P. aeruginosa in the European Region. In 2021, resistance percentages of under 5% were observed in two (5%) of 44 countries reporting data on this microorganism, whereas six (14%) countries reported percentages equal to or above 50% (see Fig. 6 in Chapter 3).
In 2021, the percentages of carbapenem-resistant Acinetobacter spp. varied widely within the Region, from below 1% in three (7%) of 45 countries reporting data on this microorganism to 50% or above in 25 (56%) countries, mostly in southern and eastern Europe (see Fig. 7 in Chapter 3).
In 2021, 11 (25%) of 44 countries reporting data on S. aureus had meticillin-resistant S. aureus (MRSA) percentages below 5% (see Fig. 8 in Chapter 3). MRSA percentages equal to or above 25% were observed in 13 (30%) of 44 countries.
Large differences were observed across the Region in the percentage of penicillin non-wild-type Streptococcus pneumoniae. Two (5%) of 43 countries reporting data on this microorganism had percentages below 5% in 2021, whereas percentages equal to or above 25% were found in five (12%) countries (see Fig. 9 in Chapter 3).
Resistance to vancomycin in Enterococcus faecium varied substantially among countries in the Region. In 2021, resistance percentages of below 1% were reported by six (14%) of 44 countries reporting data on this microorganism, while percentages equal to or above 25% were found in 17 (39%), five of which (11% of 44 countries) reported resistance percentages equal to or above 50% (see Fig. 10 in Chapter 3).
Country-specific information for each bacterial species, including information on patient age group and sex, are available on the WHO European Region website.
Antimicrobial resistance surveillance in Europe 2023 - 2021 data
English (25.75 MB - PDF)