Supporting the response to the plague outbreak in Madagascar
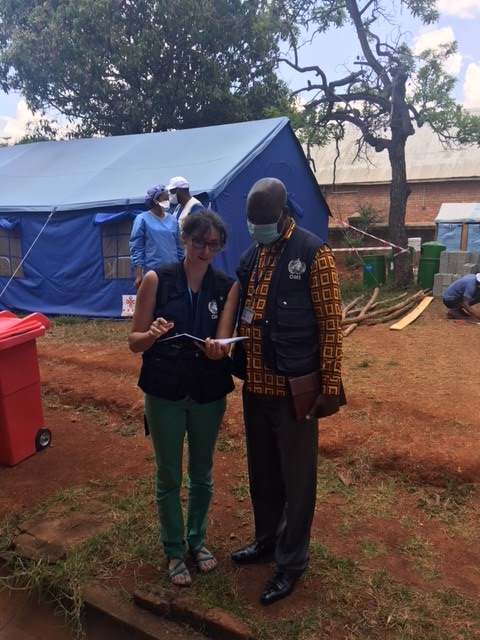
Fanny Chereau, EPIET fellow from cohort 2016, was deployed with GOARN (Global Outbreak Alert and Response Network) to support the response to the plague outbreak in Madagascar, on October 2017.
An outbreak of plague in Madagascar started in August 2017, and was notified to WHO in September. Soon after, WHO classified the event as a Grade 2 emergency, and GOARN issued a request for assistance from international partners. I was deployed as an epidemiologist to provide direct assistance to Madagascar health authorities on October 10th.
On my first day in the WHO Country Office in Madagascar, I had no idea how things would be organized, but was really excited to be part of the outbreak response. The day started with the daily Health Cluster meeting, which involved all partners in contributing to the response: Direction of Health Monitoring and Disease Surveillance, WHO, UNICEF, the Red Cross, and major NGOs, including Médecins du Monde, and Médecins Sans Frontières. I joined the surveillance platform, and worked with national and international colleagues to identify and break the transmission chains, by developing tools for contact tracing, and training the healthcare and community workers as quickly as possible.
One of the first tasks was to work with the healthcare representatives from Antananarivo health districts and from the other cities affected by the outbreak, to organize training sessions for the next 2 days.
Our team spent the evenings rapidly developing and adapting tools for contact tracing and case investigation, and preparing the communication medium, while the training sessions continued on during the day. At that point in an outbreak response, the urgency and necessity outweighs the exhaustion! The team also had to prepare communications on prevention, and transmission risks. Plague is still a terrifying disease, and the population, including healthcare professionals, were scared.

A week after I arrived, I was requested to support the laboratory response with Mr Jose Rovira Vilaplana: the combination of his 14 years’ experience in operations and logistics with WHO, and my background in biology made us the perfect team! Our job was to evaluate the capacity for plague diagnosis in the context of the outbreak, to identify how WHO could support improvements, and to implement our recommendations once validated by the incident leader and response manager. Human resources, equipment, reagents, logistics, needs for training, sensitivity and specificity of the diagnostic methods, SOPs, national regulations… We had to consider each step in the process, from the sampling of a suspected case to getting laboratory results back to the clinicians in the designated plague health centers.
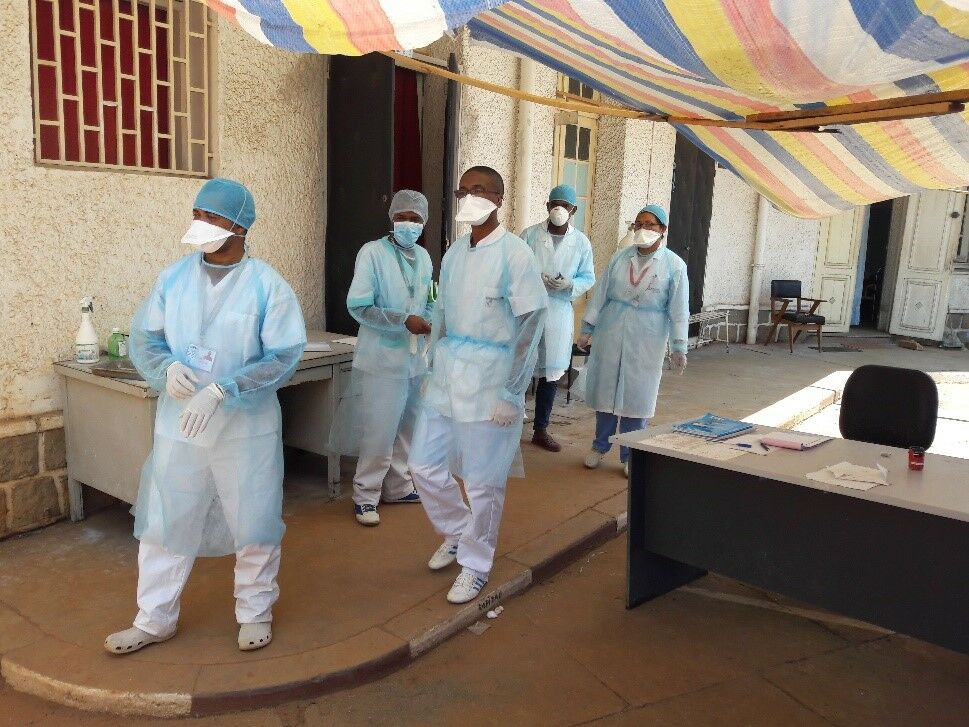
Working in lab support feels like the central hub of the public health network: an efficient laboratory can rapidly confirm or discount a clinical suspicion of plague. Rapid laboratory diagnosis with good performance is essential, particularly because the clinical picture for pneumonic plague is not specific at early stages of the disease. Laboratory confirmation is essential for the field epidemiologists to monitor the evolution of the outbreak, but also for the clinicians who take care of suspected cases.
Of course, our mission was not limited only to the short term response to the emergency: we also aimed at developing longer term solutions that will be helpful to tackle the next outbreak. We are preparing for the future, knowing that plague is endemic in Madagascar but hoping that next time, the country will have the resources to face it.

As part of WHO response team supporting the government, I had the unique opportunity to witness a public health emergency brought under control: I arrived during the peak of the outbreak and I am leaving after 5 weeks with a situation much improved. By working with epidemiologists, clinicians, community workers, communications, operations and logistics specialists, IPC specialists, and lab technicians, I had to consider issues related to clinical management, difficulties in implementing infection control and prevention measures, and how to tackle rumours effectively, so that they don’t undermine confidence in the response.
I learned a lot about crisis management, emergency response, and coordination with national authorities, political bodies and with representatives from international NGOs, in a setting where resources were limited and team members had to use all their skills and knowledge. Working across disciplines to tackle a critical public health emergency is a valuable experience that I will carry with me in my future role as an epidemiologist.
More postcards from the field
Postcards from the field
EPIET/EUPHEM fellows share their experience, read their postcards from the field






